Occupation? – Hero caregiver
In this section
Stay positive and come up with a plan
One of the most important ways to reduce stress, fear, and anxiety when taking care of
a person with schizophrenia is to MAKE A PLAN. This plan should include your
goals for recovery, daily activities for your loved one that keep them physically and mentally well, things to look out for such as relapse triggers or early warning signs, as well as how to deal with a crisis. Talk with the doctor in charge of treating your loved one about what kind of care and supervision they need, how frequently, and for how long. Make a list of all the friends and family members who can help you and be ready to adapt the plan as you go along.
Stay positive as you apply the plan on a daily basis. It will motivate you through your day-to-day challenges and will also give you hope regarding the development of new therapies that will take your loved one closer to recovery. A POSITIVE MINDSET will help you stay open to new possibilities, will increase your energy levels, and will help you prevent burnout. Having a positive attitude will also influence your loved one’s mood, improving your relationship and making their journey towards recovery easier.
STAYING POSITIVE AND COMING UP WITH A PLAN will lead to one of the most important ingredients in providing the best possible care to your loved one: a SENSE OF CONTROL.
Create a predictable environment and routine
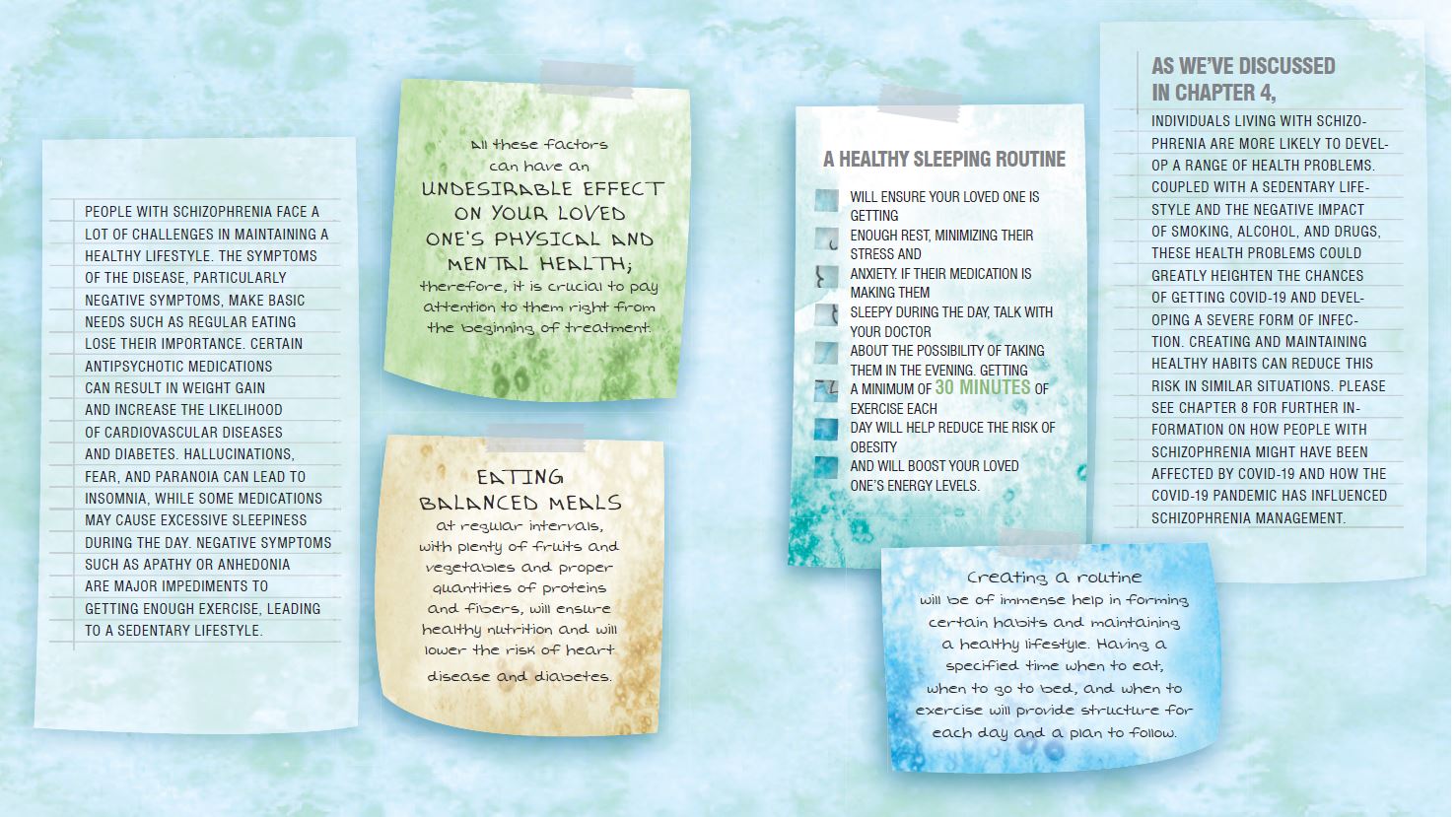
Creating a routine is immensely helpful to both you and the person you care for because
it provides stability and reliability. With consistent support and predictable routines, you both know what to expect and how to seek additional help when necessary.
Following a routine basically means PERFORMING CERTAIN TASKS REGULARLY.
For the person with schizophrenia that you take care of, a routine can encompass everything they do in a day or a week: when they get up in the morning, eat, take their medicine, go to an appointment, water the plants, or go to sleep.
Although it may appear monotonous, this type of routine MAY PROVIDE ENORMOUS COMFORT to your loved one by removing the possibility of the unexpected. When their minds are racing, they have a plan to fall back on, a pre-determined sequence of events that they can always rely on. A schedule can also help them remember to TAKE THEIR PRESCRIPTION AND GET ENOUGH SLEEP. But, more crucially, IT CAN PROVIDE AN
INTIMATE ENVIRONMENT, which can help to establish a strong basis for recovery. And when they discover their own thinking to be unclear, this intimacy might be a blessing.
A routine can also HELP YOUR LOVED ONE KEEP THINGS TOGETHER when stressful life
events bring chaos to their day-to-day life. At the time of this writing, the COVID-19 pandemic has been going on for more than 18 months, causing distress not only to those
with a mental illness but almost everyone. The unpredictability of these situations makes a
routine that maintains your loved one’s physical and mental health even more important.
To create a routine, IDENTIFY WHICH TASKS YOU NEED TO COMPLETE on a regular basis
and figure out the frequency at which these would need to be done. Using daily, weekly, or monthly checklists can help you remember what needs should be done and when. When you’ve created the list of tasks, do not forget to prioritize, making sure to complete the most important tasks first.
You can CREATE A PLAN TOGETHER with your loved one, telling them about the benefits.
However, keep in mind that they may be reluctant to get on board with the routine at first. That’s OK. GIVE THEM SOME SPACE and let them know that they are welcome to join any time. You can repeat the invitation a few times over the course of several weeks, without pressure. Even if your loved one does not take part in the routine at first, YOU SHOULD STICK TO IT because it will make your job easier, and they will also find it easier to see the benefits and join at a later time.
How you can help as a caregiver
Provide support with basic daily needs
One of the features of schizophrenia is that the day-to-day life of those who suffer from schizophrenia can become disorganized. This means that basic tasks, for example taking care of personal hygiene or getting laundry done are either completely dismissed or become an obsession, taking over the individual’s time.
This is particularly evident during the acute phase of a schizophrenic episode, as the persistent demands of the hallucinations and delusions require an overwhelming amount of energy to be satiated, diminishing one’s ability to think about anything else.
Later, in the residual phase, when they start to regain some normal functioning, daily
tasks start to become important again. In this period, THEIR BASIC LIFE SKILLS WILL NEED TO BE REFRESHED. Tasks like taking medication accordingly, shopping, cooking, cleaning, and money management have been reported to represent a challenge for people with schizophrenia in this phase.
One of your duties AS A CAREGIVER IS TO HELP THEM WITH THESE TASKS.
As you will see, many of them require you to be organized. If you are not a naturally organized person, you can develop this skill through learning. THINK ABOUT CAREGIVING AS A PROJECT: the more organized you are, the easier it is to complete it.
In fact, everything that can help you in a project – committing to deadlines, time management, breaking down large tasks into smaller ones, etc. – can also help you in caregiving.
The basic daily needs that your loved one may need your help with include:
• complying with the set time for taking medications on a daily basis;
• being consistent with regular body and hair washing, teeth brushing, and nail trimming;
• changing the bedding at appropriate times;
• cooking nutritious meals and eating them at appropriate time intervals;
• doing the laundry and housekeeping;
• grocery shopping and running errands;
• managing finances and respecting a budget;
• going on public transportation;
• scheduling appointments;
• transportation to appointments.
Some of these tasks need to be done on a daily basis, others once a week or even less frequently. Also, it is likely that you won’t have to do them every single time instead of your loved one. The fact that they need help does not mean that they are invalid or incapable.
It’s just that the illness makes it much more difficult for them to be organized and to find basic tasks important.
The main goal is to DEVELOP A ROUTINE and SLOWLY TRAIN THEM TO DO THESE TASKS BY THEMSELVES.
Create healthy habits: EATING, SLEEPING, EXERCISING
Preserve your loved one’s personal, social, and occupational functioning
Personal functioning
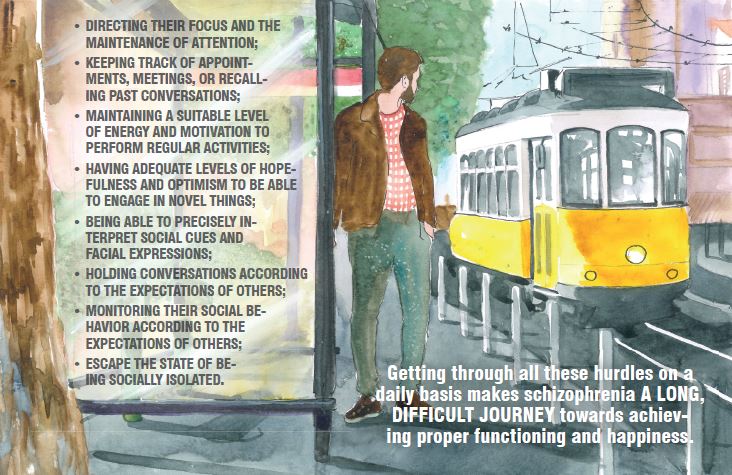
Schizophrenia is a disease that can cause your loved one to QUESTION THE REALITY OF THINGS. As a result, they may find it challenging to complete everyday ,tasks, have clear thought patterns, find solutions to problems, or make decisions.
THEY MAY FIND IT IMPOSSIBLE TO KEEP THEIR EMOTIONS UNDER CONTROL and may find it DIFFICULT TO INTERACT with family, friends, or others, such as their healthcare team.
Based on how severely the illness manifests itself, your loved one may experience difficulties with skills such as:
Social functioning
One of the distinguishing aspects of schizophrenia is SOCIAL DYSFUNCTION, and many people living with the disorder find it difficult to interact with others, even when their psychotic symptoms are under control. As a result, for people with schizophrenia, the illness can become a constant struggle to figure out HOW TO FIT INTO SOCIETY.
In this regard, the most debilitating symptoms are PARANOIA AND DELUSIONS. The belief that others are trying to hurt them or are thinking bad things about them makes it very difficult for people with schizophrenia to have a dialogue or keep their calm in any kind of social situation.
One of our most important social interactions is, of course, establishing a romantic relationship with another person. Generally, people aspire to form romantic relationships
and start a family. However, a serious, long-term illness, like schizophrenia brings along a SERIES OF PARTICULAR DRAWBACKS, which makes it troublesome to form and maintain close relationships.
The most significant of these drawbacks is THE NEED TO ADAPT TO THE ILLNESS, which may cause alienation in the relationship due to the presence of stigmatization and self stigmatization. The stigma of schizophrenia leads to a vicious CYCLE OF SELF-STIGMATIZATION AND ISOLATION, decreasing social functioning, which in turn amplifies the stigma. Self-stigmatization also leads to low self-esteem. As a result, the large majority of people with schizophrenia have the belief that others do not have the desire of being with a partner diagnosed with such illness. Hence, schizophrenia results in a reduced prospect of getting married, particularly for men, and an increased risk for broken marriages regarding women. Love relationships are also COMPLICATED BY INTERNAL OBSTACLES, described by people with schizophrenia as losing a part of themselves, modifications to the experience of emotions, and challenges with accepting alternative beliefs.
They also report diminished trust towards others but also themselves, as well as towards their own memories, feelings, perceptions, and desires.
There are also more practical challenges. Schizophrenia (and certain antipsychotic medications) may cause people to become less interested in sex. Some antipsychotics can cause weight gain, while the person taking them may FEEL UNATTRACTIVE. For people who have had schizophrenia for many years, poverty can also become a roadblock in creating and sustaining relationships.
All these difficulties might lead to the belief that love and schizophrenia are not compatible. However, regardless of the chaos in their minds and the lingering impact of psychotic experiences, most people with schizophrenia have the ability to communicate nuanced feelings and outlooks towards love.
THEY NEED TO LOVE AND TO BE LOVED.
They have a strong desire for meaningful relationships, romance, and family. It’s just that the illness does not allow their self to express the full extent of its potential. Although it means a lot of work, if the disease of your loved one is kept under control, establishing a romantic relationship with someone who accepts them as they are can have a huge positive impact on their life.
Occupational functioning
People with schizophrenia are known to have a LOWER PERFORMANCE IN WORK-RELATED TASKS as a result of their altered cognitive functioning and negative symptoms
When the illness is not adequately controlled by medication, it can severely affect both
their PHYSICAL AND MENTAL WORK CAPACITY. Hallucinations can make physical
work impractical and can be dangerous for your loved one but also for others in the
workplace. Most people with schizophrenia will also struggle with DISORGANIZED THINKING, SPEECH, AND BEHAVIOUR, symptoms that make it very difficult to function in a work environment.
The first symptoms of schizophrenia usually appear around the age when individuals are attending college. This period in their life can be marked by a psychotic episode, and it is natural for this event to be considered the end of what was supposed to be a successful life. But the reality is different and if symptoms are successfully controlled, enrolling back into education or getting a job may be UTTERLY POSSIBLE.
It is in our nature as humans to have a better feeling about ourselves when we are engaged
in useful tasks. Your loved one is also able to pursue their life goals, a journey that has a
significant impact on their recovery. WORKING IMPROVES THEIR SELF-CONFIDENCE AND GIVES THEM A SENSE OF BELONGING, INCREASING AT THE SAME TIME THE QUALITY OF THEIR LIFE.
When looking for a job, one of the major impediments in the case of people with schizophrenia is not having a clear idea of where to begin. Many of them possess minimal to
no work experience at all and are not able to make out the nature of work they would be capable of pursuing. Therefore, it is very important to make sense of what they excel at by observing their PERSONAL QUALITIES and also to have a good understanding of the current job market prior to the job hunt. However, most individuals with schizophrenia have the willingness and ability to flourish in their workplace if they find a job that matches their interests, acknowledges their strengths and skills, and is accommodating to them.
LIVING WITH SCHIZOPHRENIA DOES NOT IMPLY THE IMPOSSIBILITY OF HAVING
A CAREER OR SUCCESSFUL LIFE. As long as there is a positive treatment response, it
is highly probable that people can accomplish whatever it is that they aspire to.
Assist with therapy and progress tracking
A person with schizophrenia will almost certainly be recommended prescription medication.
As a caregiver, you may find yourself involved in tasks that include:
• picking up prescriptions;
• keeping a record of the use of medication;
• paying attention to side effects and reporting these to the doctor or psychiatrist;
• encouraging your loved one to take their medication at regular intervals;
• using a preplanned schedule to keep track of the medication use;
• encouraging the use of a pillbox or timer;
• assisting with long-acting injection type medication;
• consulting with the doctor regarding possible drug interactions;
• keeping a register of which medications and supplements are being taken;
• taking care that other substances, such as drugs or alcohol are not combined with the medication;
• keeping notes of medication to assess which one is personally more effective;
• keeping track of why some of the medications were changed.
TAKE SIDE EFFECTS SERIOUSLY. After noticing side effects, a vast number of individuals with schizophrenia quit taking their medication. A better alternative would be to bring up the undesired side effects to the doctor’s attention, who can either reduce the dose, prescribe a different antipsychotic, or add another medication to combat specific side effects.
ENCOURAGE YOUR LOVED ONE TO TAKE MEDICATION REGULARLY.
Even if the side effects are controlled, individuals with schizophrenia may reject their medication or simply find it difficult to remember when and how much of it to take. In such cases, they might find it helpful to install medication reminder apps, make use of weekly pillboxes and keep calendars on hand.
BE CAREFUL TO AVOID DRUG INTERACTIONS.
In order to prevent your loved one from any drug interactions, present the doctor supplements that they take. Combining schizophrenia medication with either alcohol or illegal drugs can cause serious harm.
In case the person you take care of has a problem with abusing substances, it is important to inform the doctor about it.
TRACK YOUR FAMILY MEMBER’S PROGRESS. A good way to monitor the changes in behaviour and other symptoms your family member experiences as a result of taking medication are mood tracking apps, journal entries, and keeping a diary.
Your loved one may also attend cognitive behavioral therapy or social skills training. Your
responsibility as the caregiver could be assisting them with their commute to therapy, ensuring they keep their therapy ongoing, or helping them with homework tasks. When KEEPING TRACK of your loved one’s adherence to treatment and their overall progress, it is easy to become overprotective.
Make sure you RESPECT their privacy and personal boundaries. By giving them responsibilities (e.g., to take their medicine every day at the specified time), you are empowering and motivating them, providing a sense of purpose in their life.
Staying on track with medication
Ensuring that an ill person takes their medication regularly and consistently is called “COMPLIANCE” or “ADHERENCE”.*
Although it doesn’t seem too difficult, compliance is actually one of the most challenging factors for long-term treatment in any type of illness.
In schizophrenia, the problem of non-compliance is significant: only 58% of patients collect their medication in the first 30 DAYS after hospital discharge, and only 46% continue their initial treatment for 30 DAYS or longer. This high rate of non-compliance can be explained by poor insight into the illness, cognitive problems, side effects, and substance abuse associated with schizophrenia. Stressful events that turn their lives upside down for long periods of time, such as the recent COVID pandemic and the restrictions that came with it, can also make it more difficult for them to take their medicine consistently or attend therapy appointments. Also, many people with schizophrenia do not recognize they are ill; hence they don’t understand why they need medication. Figuring out the appropriate dose or combination is usually TIME-CONSUMING, and it’s a difficult process that can lead persons with schizophrenia to abandon treatment altogether
Being compliant, not just with medication but the entire treatment plan is very important for
overall success. As a caregiver, one of your MAIN RESPONSIBILITIES IS MAKING SURE THAT THE PERSON YOU CARE FOR:
• takes medication consistently;
• attends appointments on a regular basis;
• engages themselves in counseling and group therapy;
• informs the doctor about their experiences;
• asks for help from their support group if in need;
• has patience with themselves as well as their providers;
• reminds himself/herself that they are on a journey.
If you find out that your loved one has trouble keeping up with their medication, try to find the cause behind their non-compliance. Are they feeling better and think the treatment is not needed anymore? Do they think the treatment doesn’t work? Are they concerned about the side effects? Or is it because of a lack of routine? Make medicine-related decisions with your relative’s doctor or the care team that is caring for him or her. In this manner, you can all build a trusting environment in which your loved one feels comfortable sharing how and what they are feeling.
When a person with schizophrenia stops taking their medication, there is a VERY HIGH RISK OF A RELAPSE. This involves the return of psychotic symptoms, and the sudden interruption of treatment might cause significant adverse effects such as headaches, depression, anxiety, and suicidal thoughts. Talk to the doctor treating your loved one if you see they are thinking about or have already stopped taking their medication
Tackle substance abuse and addiction
Individuals living with schizophrenia may experience a lot of LONELINESS, DEPRESSION,
and FRUSTRATION due to the fact that their feelings and actions differ from those of others. Stress, anxiety, and prolonged isolation, characteristics of the recent coronavirus pandemic, may accentuate these feelings and their impact on your loved one’s quality of life. In these circumstances, it is somewhat understandable that they try to find relief in substances that CAN LEAD TO ADDICTION.
These can include anything from alcohol and nicotine to coffee, energy drinks, and drugs. Some of these substances, such as alcohol or marijuana, alleviate boredom and make it easier to forget about the illness for a short period of time, but cause hangovers or paranoid thoughts the following day. Others, such as coffee and energy drinks, are often used to overcome negative symptoms and sleepiness during the day, but CAN ALSO CAUSE INSOMNIA, leading to a vicious circle.
Statistical data suggest that around half of people with schizophrenia suffer from alcohol
and drug dependency, while over 70% of them have nicotine dependence.
An important thing to note is that there is a DIFFERENCE BETWEEN ABUSE
AND ADDICTION. When the use of a substance interferes with work and social relations, affects the user’s health, or causes danger, we are talking about substance abuse. When the substance causes physical dependency, and the user has difficulties controlling its use,
we are talking about addiction.
The impact of substance abuse is substantial, both on the user and their family. Alcohol and drugs worsen the symptoms of schizophrenia and increase the risk of a relapse. The use of these substances also interferes with their daily activities, generates conflicts in their relationships, and can get them into trouble with the law. Family members usually find it very difficult to accept that their loved one does not have any control over alcohol or drugs, and they are faced with feelings of frustration, anger, helplessness, and despair. They may also feel increased fear and insecurity, as substance abuse can lead people with schizophrenia to become hostile, withdraw socially, or even attempt suicide. It is essential that you try to UNDERSTAND the cause and approach them with deep understanding and compassion because substance abuse is usually a sign of suffering. They are not doing it because they are a bad person or because they are trying to hurt you or themselves.
They are doing it because they are TRYING TO FIND AN ESCAPE, a way to alleviate their anxiety and depression. However, these substances provide only short-term relief, and the addiction adds to their stigma and suffering.
Overcoming addiction is a gradual, complex process that requires acknowledging the problem, motivation, behaviour changes, and help in achieving a healthier lifestyle.
You can have a significant role in this process by empowering your loved one and providing them with a sense of purpose.
Talk to the doctor in charge of the treatment if you think your loved one is struggling with substance abuse or addiction.
In severe cases, detoxification or hospital admission may be needed to get your loved one back on track.
What to do in different phases of the disease
The manifestations of schizophrenia can be markedly different in different phases of the disease and different approaches are required from you as well.
The active phase
The active phase, more specifically a psychotic episode, can cause a lot of stress
and confusion for both you and your loved one. Due to the variety of symptoms, THERE ARE NO GOLDEN RULES IN THIS PERIOD. The most important thing you can do is try to UNDERSTAND what your loved one may be experiencing. The hallucinations and delusions are very real to them. Do not get involved in long debates trying to convince them of the contrary, because this will make them feel like they cannot tell you what they are going
through. USE EMPATHY, not arguments. Show your concern while steering clear from confrontations and restraining from being critical of or putting the blame on them.
Remember that most of what you see in this period is a MANIFESTATION OF THE DISEASE. Just listen and let them know that you understand that they must experience a lot of fear, frustration, and anger. Try to minimize their stress and provide a peaceful atmosphere that can help them recover.
When your loved one is experiencing hallucinations and delusions, they may need a lot of personal space and may feel uncomfortable being around other people. Usually, the positive symptoms do not stop suddenly, even with proper treatment. In this period, you may feel that you need to let them rest and do everything yourself.
However, keep in mind that REBUILDING THEIR CONFIDENCE is very important for recovery. Encourage and support your loved one as they take on daily responsibilities, and let them know that you are there for them when they need help.
The residual phase
After a psychotic episode, your loved one may need a QUIET PLACE AND A LOT OF REST. The transition to a state where the symptoms are mostly subdued can be shorter or longer; some people can get back to their usual routine fairly quickly, others need considerable time and effort to do so. During this time, it may be difficult for the family to cope with negative symptoms such as avolition or anhedonia.
As mentioned before, it is important to remember that THEY ARE PART OF THE ILLNESS and do not mean that the person you take care of is unwilling to get better.
With proper treatment, YOUR LOVED ONE WILL BE ABLE TO START TO TAKE ON MORE RESPONSIBILITIES. It is important to START SLOW and let them ease into them at their own pace. You can start with tasks related to personal hygiene, getting dressed, or doing household chores. With time, you can start to encourage social interactions, for example by inviting one or two friends over for dinner.
DO NOT FORCE your loved one to participate if they do not want to, and always make sure to provide a possibility to tone things down if they become anxious. You can also initiate going out for a walk in a quiet part of the city or spending some quality time listening to music or playing cards.
Remember that you are the person that your loved one spends most of their time with and their closest ally in their battle with schizophrenia. Respect, patience, and compassion will be remarkably valuable at helping both of you be in control of the illness and starting to live life to its full potential once again.
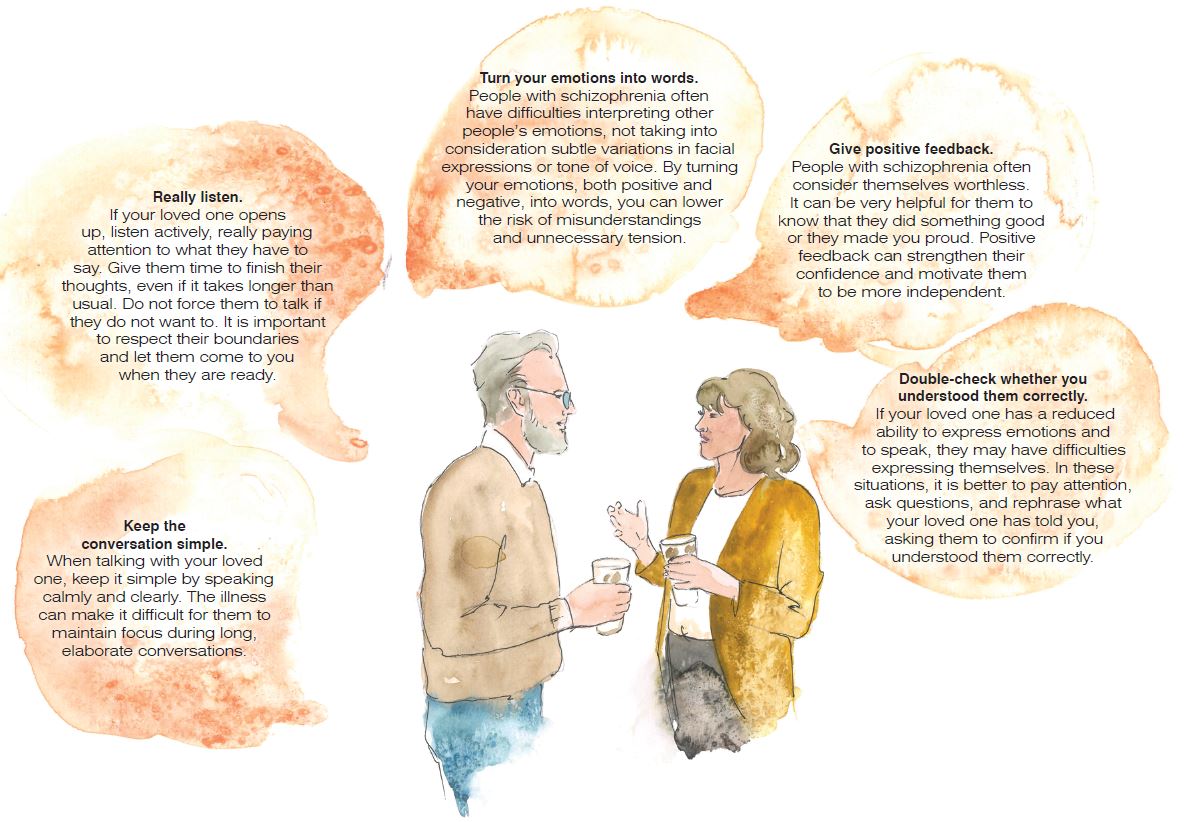
How to communicate with your loved one
Communication is an essential part of human relationships, especially when family is
concerned. Schizophrenia can make it DIFFICULT TO COMMUNICATE with your loved one, posing a set of very specific challenges.
These challenges CAN BE OVERCOME, however, by understanding how the illness impedes your loved one’s ability to communicate.
Basically, almost all manifestations of schizophrenia can lead to difficulties in communication: cognitive dysfunction can make it hard for them to focus or remember what you were talking about; hallucinations and delusions change their reality and can make any attempt of inserting logic into the conversation futile; negative symptoms, such as flat affect or apathy, can make it difficult for you to interpret their emotions.
Good communication is very important in a chronic mental illness where all family members must work together to minimize the symptoms. You can IMPROVE COMMUNICATION with your loved one by abiding by a few simple rules:
Good communication will REDUCE YOUR LOVED ONE’S STRESS, leading to better treatment outcomes and a lower risk of relapse. It will also lower the stress among the family members, will improve family relationships, and will reduce the risk of burnout.
Talking about your emotions
As the caregiver of a person with schizophrenia, you may be burdened with feeling UNCERTAIN, SHAMEFUL, GUILTY, and ANGRY. Similarly to the person you are taking care of, you may feel stigmatized and socially isolated. Also, having the role of a caregiver on top of your existing roles in the family may provide additional stress, both psychologically and economically.
From your position, it is natural for stress to lead to negative attitudes and behaviours towards your loved one, such as aggression and cynical comments, and you may even get over-involved in their life. These attitudes and behaviours are collectively known as EXPRESSED EMOTION and CAN HAVE A NEGATIVE IMPACT on your loved one’s illness. People with schizophrenia who live in family circles with high levels of expressed emotion have a higher risk of relapsing.
You can avoid letting your stress and tiredness take a toll on your relationship by TALKING ABOUT YOUR FEELINGS with the person you care for. As we’ve mentioned before, expressing your emotions is very important in coming to terms with the illness and can have significant benefits for both of you. Let them know that YOU ALSO NEED SYMPATHY AND EMPATHY. Rather than making accusations and leaving them with the feeling that they are a burden, talk about your emotional needs.
Ease the emotional impact of schizophrenia
Set goals and celebrate success
Creating a plan that will help your loved one on their journey to recovery also means
holding on to some clear goals to GUIDE both of you along the way. Some of these goals CAN BE SMALL, like getting your loved one to take their medication each day.
Other goals CAN BE BIG, like continuing school or getting a job. When setting these
goals, it is very important to calibrate your expectations based on how severe the symptoms
are and at what stage the disease is.
You also have to be aware of your own limitations. CAREGIVING IS LIKE RUNNING A MARATHON: giving your all in the first few miles will quickly lead to exhaustion and will force you to give up the race. Set these goals together with your loved one, and celebrate success each time you reach a goal. It will boost your motivation and will make it easier to keep the next goal in sight. CELEBRATING SMALL WINS will also help you achieve the bigger goals and will give you both energy to continue your journey.
Make decisions together
Although the disease often causes chaos in their minds and interferes with their ability
to make decisions, PEOPLE WITH SCHIZOPHRENIA ARE NOT INCAPABLE. However,
they often have low self-esteem and do not consider themselves worthy of anyone’s
attention. Involving them in the decision-making process can ENHANCE THEIR AUTONOMY AND EMPOWER THEM to participate more actively in their treatment.
Make all kinds of decisions together, small and major, from what to eat or what movie to see, to developing a daily routine or discussing how their treatment is coming along. Making decisions together is a process of mutual acceptance and shared responsibility that places you and your loved one on the same level, making them feel IMPORTANT AND RESPECTED.
Deal with your loved one’s emotions
For people with schizophrenia, the illness can be an EMOTIONAL ROLLERCOASTER. The abundance of negative emotions makes them feel less human, adds to their burden, and increases self-stigmatization.
As the disease changes certain processes in the brain, they find their environment to be habitually OVERWHELMING, their thinking may be OUT OF ORDER, and they may have DIFFICULTIES IN EXPRESSING THEIR EMOTIONS. The latter is actually one of the most debilitating and treatment-resistant symptoms of schizophrenia.
One of the most important ways you can cope is to continue to GAIN KNOWLEDGE regarding the condition, as well as what experiences your loved one will face.
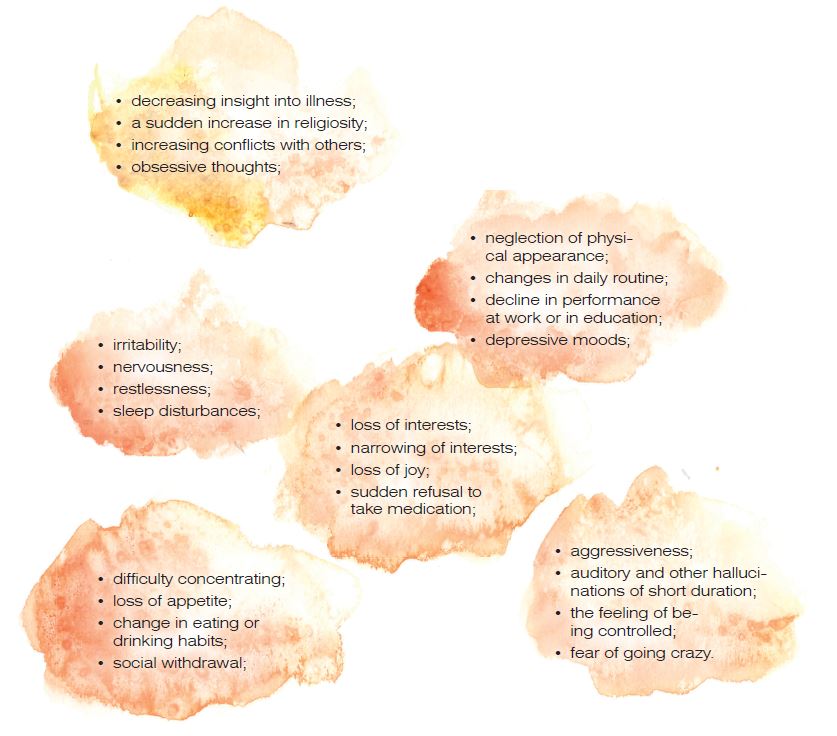
Relapse and crisis
The course of schizophrenia is usually EPISODIC, with symptoms of varying severity. When your loved one’s symptoms WORSEN AFTER A PERIOD OF FEELING BETTER, it is called a “relapse”. The majority of people with schizophrenia experience multiple relapses during the course of the illness. As a caregiver, you have a very important role in WATCHING FOR THE
EARLY WARNING SIGNS.
This process is similar to setting up a light connected to a motion detector. If you set the detector’s sensitivity too high, the light turns on even when you don’t need it, wasting energy. If you set it too low, the light does not turn on when you need it, and you have to walk in the dark. Watching out for relapse is about calibrating your “EMOTIONAL DETECTOR” to find the right BALANCE between being overprotective and not paying enough attention to the warning signs.
A person with schizophrenia will usually show similar signs before each episode of psychosis. Thus, the symptoms and events that occur during the first episode can significantly help you in identifying specific signs in the days or weeks before the relapse. Knowing how to IDENTIFY A RELAPSE and what to do in a crisis will give you a SENSE OF CONTROL and will help you in overcoming this stressful period.
How to identify a relapse
The discontinuation of taking medication is the most common factor for relapses in schizophrenia, therefore, it is crucial that your loved one carries on with TAKING
THEIR MEDICATION AS INSTRUCTED. Despite the fact that relapses may take place even in the event of compliance with prescribed medication, recognizing early warning signs and taking instant action may help you counteract a full-blown crisis. Frequent warning signs of schizophrenia relapse include:
IMPORTANT NOTE! IT IS NOT NECESSARY FOR ANY OF THESE SIGNS TO INDICATE THE BEGINNING OF A PSYCHOTIC EPISODE, due to the fact that some may be associated with physical illness, work or school-related stress and pressure, or issues with important relationships.
Moreover, these signs do not necessarily occur at once; they usually appear over a course of several days or weeks, or they are not present at all. SMALL CHANGES IN THINKING, MOOD, OR BEHAVIOUR MAY OFTEN GO UNNOTICED or seem insignificant, being recognized as warning signs only after the relapse had taken place.
Also, you may notice other signs that are not on this list. In time, you will be able to compile YOUR OWN LIST BASED ON THE SIGNS YOU OBSERVE together with your loved one, and you can learn together how to recognize an impending relapse.
The main goal of looking for warning signs is to act quickly in order to PREVENT RELAPSE
AND AVOID HOSPITALIZATION. If you observe several of the signs listed above, try to find the cause.
Has your loved one been taking their medication regularly? Have they been recently using
alcohol or drugs?
Have they experienced high levels of stress lately?
Are they eating, sleeping, and exercising properly?
If none of these factors can be accounted for, consult with their doctor whether their
medication dose should be increased. In any case, follow the warning signs closely, even after you have taken measures until you can see clear improvement. If the warning signs do not regress shortly or if they get more prominent as time passes, call the doctor treating your loved one.
How to prepare for crises
Even when you do everything possible to avoid a relapse, there may be occasions
where the condition of the person you care for declines quickly, and hospitalization is needed to ensure they are safe and treated optimally. A pre-arranged emergency plan may help with handling a crisis in a safe and swift manner in the case of an acute psychotic episode. An adequate emergency plan for someone living with schizophrenia may involve
several or all of the following items:
• phone numbers of the therapist, psychiatrist, and other healthcare providers treating your loved one;
• the phone number and address of the hospital mapped out for psychiatric admission;
• phone numbers of who would be helpful in a crisis, such as family members or friends;
• addresses of emergency rooms or walk-in crisis centers;
• your own contact details such as phone number and address;
• the diagnosis and medications of the person you care for;
• known triggers;
• known early warning signs; history of drug use;
• previous psychoses or suicide attempts;
• things that have helped in the past;
• a plan on how to deal with acute psychosis;
• a plan to get them help.
You can add or remove items from this list based on your own experience.
Together with your family, you can also create a more specific plan based on your loved one’s symptoms and disease course. This plan should be individualized as much as possible, and everyone involved should feel comfortable with it. In this plan, you can specify what kind of signs to watch out for, who will contact whom and when, and for what purpose.
DISCUSS THE EMERGENCY PLAN with the person you care for and the doctor involved
in their treatment. It is very important to discuss the plan with your loved one at times
WHEN THEY ARE NOT IN A STATE OF CRISIS. This would ameliorate the feeling of threat in case you do encounter such situations. Make sure to obtain their permission to call the doctor or do whatever is necessary to keep the crisis under control. Also, make sure you obtain a so-called RELEASE FROM SECRECY while their condition is stable. This document enables your loved one’s doctor to share important information with you in case of an emergency. For more information, please see the LEGAL ASPECTS SECTION at the end of the chapter.
KEEP COPIES of the plan in multiple locations. Keep a print in a kitchen drawer, the glove compartment, your smartphone, your wallet, or on your bedside table. In the event of a psychotic episode, your loved one’s symptoms may make it difficult for them to understand that you want to help, and they may feel threatened or even become violent. For these situations, keep a copy of the plan in a room that has a lock and a phone. This will enable you to contact your doctor in a safe environment.
How to handle a schizophrenia crisis
As a person taking care of someone with schizophrenia, it is essential to be aware of WHAT YOU CAN DO IN CASE OF A CRISIS. Below are several tips on what to do in this situation:
Remain calm.
• Remember that what you see during a crisis is not your loved one, but the acute manifestation of a severe illness.
• Remember that you cannot reason with acute psychosis.
• Remember that your loved one may be frightened by the feelings they experience or by the inability to be in control.
• Reduce distractions by switching off the TV, PC, bright lights that might emit sounds, etc. Request that any casual visitors make their way out; the fewer people are present the better.
• Take a seat and ask them to do the same.
• Avoid direct, continuous eye contact.
• Avoid touching your loved one.
• Speak in a low voice and a calm manner, avoid shouting or threatening them.
• Validate their fears.
• Do not argue about their delusions.
• In case you feel irritated or angry, avoid making these feelings obvious.
• Abstain from sarcasm as a weapon.
• Gently redirect the conversation to safe topics.
• Contact the doctor treating your loved one.
What to do when your loved one intends to hurt themselves
Although it can be frightening to think about your loved one hurting themselves, you have
to be aware that people with schizophrenia have an INCREASED POTENTIAL for depression
and suicidal thoughts. As such, you need to take very seriously any gestures and threats that may appear related to self-harm. SUICIDAL IDEATIONS, also known as thoughts or comments about suicide, may appear minor initially, such as “I wish I was not here” or “Nothing matters”.
However, as time passes, they may progress and become evident and dangerous. There are several SIGNS THAT MAY INDICATE THAT YOUR LOVED ONE HAS SUICIDAL THOUGHTS: severe depression, the feeling that nothing has meaning or value anymore, or a bleak outlook into the future. Hallucinations are also often associated with suicidal thoughts, especially if there are voices telling your loved one to hurt themselves.
TAKE IT SERIOUSLY EVERY TIME your loved one mentions death or suicide, even if it is only a passing reference or a joke. In case of a suicide-related crisis occurrence, family members and friends are frequently taken by surprise, being unprepared and not certain of what to do. Individuals experiencing a crisis may act unpredictably, with striking changes in their actions. The following tips can help you in handling a suicide crisis:
• Keep calm and practice patience.
• Communicate in an open and honest manner. Don’t hesitate from asking direct questions like: “Do you have a plan for how you would kill yourself?”
• Remove any items from their environment that they would use to hurt themselves such as knives, guns, or pills.
• Ask short and direct questions in a peaceful manner, such as “Can I help you call your psychiatrist?”
• In the case of several people surrounding them, only let one of them speak at a time.
• Convey your concern and support.
• Don’t argue, threaten them or speak in a different tone.
• Do not dispute the idea of the rectitude of suicide.
Let your loved one know that they are able to discuss what they are going through with you if they struggle with suicidal ideation. Ensure that they have an OPEN AND COMPASSIONATE APPROACH when they talk to you. Rather than proving their negative statements wrong, try to ACTIVELY LISTEN TO THEM, be reflective about their feelings and provide them with an overview of their thoughts. By doing this, you can help your loved one feel like they are listened to and validated. Don’t let fear prevent you from talking to them about how they feel, whether they feel safe or if they experience thoughts related to self-harm. HAVING A CONVERSATION ABOUT SUICIDE DOES NOT MAKE IT MORE LIKELY TO HAPPEN; it lets your loved one know that you care about them and makes prevention actions possible. Remind them that mental health professionals have training in how to provide help with understanding their feelings and improving their mental well-being. More importantly, let them know that suicidal thoughts are part of the disease; THEY ARE A SYMPTOM, and similarly to other symptoms, THEY CAN GRADUALLY IMPROVE WITH TREATMENT.
Address medical and/or healthcare professionals for assistance right away in case you think your loved one could harm themselves. Although you may feel that you are betraying their confidence by sharing their innermost thoughts, it is more important to ACT IN THEIR BEST
INTEREST and SHARE THE INFORMATION with a healthcare professional.
If you are unsure about when to call the doctor, DO IT SOONER RATHER THAN LATER.
Talk to a healthcare professional even when there is only ideation. Whenever there is a crisis, involve the doctor treating your loved one and discuss how to handle the situation. They will know how to assess the risk of your loved one hurting themselves.
Similar to a psychotic episode, make sure to obtain a release from secrecy for the doctor before the actual crisis occurs.
At the doctor’s office
Even if it appears uncomfortable from time to time, EFFICIENT COMMUNICATION BETWEEN THE DOCTOR, THE PERSON WITH SCHIZOPHRENIA, AND YOU – THE CAREGIVER IS VERY IMPORTANT. Accompany your loved one to their appointments. Receiving information directly and in-person is favorable as it lets you know what to expect and how to prepare for it.
Keep in mind, however, that there is a chance your loved one may prefer you not to come with them, particularly during the initial few visits. It is important to RESPECT THEIR WISHES, however, in case things change make sure to be there for them. It is essential to develop A TRUSTFUL ATMOSPHERE that will make everyone’s job much easier.
When face-to-face visits are not possible, you can use phone calls, emails, or video chat to discuss with the doctor treating your loved one. The COVID-19 pandemic has greatly increased the popularity of TELEMEDICINE because it allowed patients to consult their doctor without leaving their house and becoming exposed to the coronavirus. With the exception of acute or severe cases, telemedicine is invaluable in ensuring the continuity of care.
As the caregiver of your loved one, you have significant insight to share. DO NOT BE AFRAID TO RAISE CONCERNS, ASK QUESTIONS, and BE OPEN about discussing all the options out there.
How to prepare for an appointment
In preparation for the appointment, comprise a list of the following:
• the symptoms experienced by your loved one, even if seemingly unrelated to the appointment matter;
• essential personal information, taking into account considerable stresses and current life changes;
• the medications they are taking, as well as vitamins and supplements,
including the dosages; also include information on which medication worked and which didn’t. If a medication was changed recently, include the reason for changing it;
• information regarding substance abuse, addiction issues, or recent lifestyle changes;
• questions to ask the doctor.
Enter your and your loved one’s ups and downs regularly in a diary. Based
on the things you note in this diary, write down the answers to the following questions before your appointment:
• How do you feel about the overall management of their condition?
• Does your loved one achieve the expected results from the prescribed treatment?
• What is their opinion on their progress through this journey?
• What effects does their medication have on them, and do they experience any side effects?
• Do they take their medication as prescribed, and do you think they ever say they have taken it when they haven’t?
• Do they ever stop taking their medication when they feel better/ill?
What to ask the doctor
Some basic questions to ask the doctor include:
• What treatment options are there?
• What can we anticipate short and long-term (symptoms as well as possible medication effects and related side effects)?
• What available support and services can we make use of?
• How can I make myself as supportive and helpful as possible?
• Have you got any leaflets or other printed resources you could give me?
• Are there any online resources that you would suggest?
DO NOT HOLD BACK FROM ASKING ANY OTHER QUESTIONS regarding your loved
one’s symptoms, treatment, challenges, or overall progress.
BE AS SPECIFIC AS POSSIBLE. The doctor may also inquire information regarding the symptoms displayed by your loved one, daily functioning, and response to therapy. Getting involved in the conversation will make it much easier for both of you to ensure your loved one is on the right path to recovery.
Financial, legal, and housing-related aspects
Financial aspects
People with schizophrenia often have a reduced ability to function independent-ly in the community. As a consequence, THEIR FINANCIAL CAPACITY – the ability to manage their own money and financial affairs – CAN ALSO BE REDUCED. The reasons are pretty straightforward: often, the onset of schizophrenia occurs at such an early stage in their life, that many of them simply do not have the chance to acquire basic financial skills and experiences. The unfavorable consequences of positive and negative symptoms, as well as the cognitive disturbances associated with the disease also hamper this process.
The reduced financial capacity of people with schizophrenia CAN HAVE A NEGATIVE IMPACT on their well-being, creating barriers to recovery, and also on their family relationships. The repercussions differ to a great extent depending on the person. It may include a decreased ability to earn an income, being incautious with their money, or being susceptible to being used for their funds by their own acquaintances or family members. In severe cases, the consequences can be devastating, leading to malnutrition, substance abuse, and even homelessness. People with schizophrenia can spend large amounts of money on addictive substances and many of them dissipate their monthly aids intended to support themselves. As a result, MONEY MISMANAGEMENT IS A KEY CONCERN for their family members.
When a person with a severe mental illness is deemed unable to be in financial control, they may be restricted from having access to their finances. For some, this may mean that a power of attorney is arranged. For more information on power of attorney, please see the legal aspects section below. It may be necessary to appoint someone else to REPRESENT THE PAYEE if the payee’s income comes from disability benefits. Payees receive the disability benefits instead of the person with a mental illness and ensure that their needs are fulfilled, including those for nutrition, housing, and medication bills. In most cases, the payee of someone living with a severe mental illness is a family member.
Having a payee has NUMEROUS BENEFITS for people with schizophrenia, such as more stable circumstances, reduced or no consumption of alcohol, drugs, and other damaging substances, and even a constant pace with respect to therapy.
Payee arrangements are also ASSOCIATED WITH REDUCED HOSPITALIZATION AND
HOMELESSNESS, as well as increased ad-herence to treatment. However, this kind of relationship has also DRAWBACKS. Since people with schizophrenia are usually less motivated to seek employment when receiving disability benefits, not having control over their own money can further increase their dependency. Having someone else control
their money can also lead to CONFLICTS, money affairs being one of the main causes of disagreements within the family. People with severe mental illnesses are more inclined to display aggression towards their caregiver in cases where the latter is in control of their finances. Conflicts can also arise when the person with a mental illness feels that the payee has too much control or that spending decisions were forced on them.
Even if you are not formally appointed as a payee, your responsibilities as a caregiver may include taking care of your loved one’s finances.
Depending on their condition, you can TEACH THEM SOME BASIC FINANCIAL SKILLS, such as how to set up a budget or how to save money, which will help them become more independent in the long term.
Legal aspects
There are several different legal aspects that might come up in your relationship with the person you care for, depending on the severity of the disease and the ex-
tent to which it limits their capacities.
GUARDIANSHIP. Guardianship can be defined as the legal process used to certify that individuals incapable of making decisions by themselves have someone explicitly assigned to make these decisions in their name. The person who has an assigned guardian is called a “WARD”. A guardian has the responsibility of offering the ward care and comfort; THE COURT IS LIABLE FOR ADJUSTING THE GUARDIAN’S POWERS BASED ON THE WARD’S DISPLAYED NEEDS. Additionally, in order for the ward to revert to caring for themselves at the earliest opportunity, the guardian shall secure services in support of that.
The ward is entitled to oppose the guardianship, the guardian’s powers, and the appointment of a certain guardian.
ENSURING CONTINUITY OF CARE. Although it can be an awkward or uncomfortable subject, once you have become the caregiver of a person with a chronic mental ill ness, you should start thinking about WHO WILL TAKE OVER YOUR CAREGIVER DUTIES WHEN YOU GET SICK, GROW OLD, OR DIE. Consult with an attorney and make sure to prepare the legal documents in time. It is important to note that the decision regarding your replacement is yours only if you have guardianship over the person you take care of. Otherwise, you both have equal rights, and your loved one can also make this decision. Even if you are not a guardian, thinking about who can replace you should be a natural step in your relationship.
DECISION-MAKING CAPACITY. This capability may be characterized as one’s ability to make reasonable judgments, which necessitates the acknowledgment, evaluation, and interpretation of data. Because of their impaired cognitive functioning, PEOPLE WITH SCHIZOPHRENIA MAY BE LESS ABLE TO MAKE TREATMENT DECISIONS.
RELEASE FROM SECRECY. In most countries, medical professionals are bound to secrecy. This means that they cannot share information about their patients or their condition with other individuals, not even to the family members of the patients.
When you are the caregiver of a person with schizophrenia, THE PERSON CAN SIGN A DOCUMENT THAT RELEASES THE DOCTOR FROM THE BOUNDS OF CONFIDENTIALITY AND ALLOWS THEM
TO SHARE INFORMATION WITH YOU, the caregiver, in the event of an emergency.
POWER OF ATTORNEY. A power of attorney is a legal instrument that authorizes anoth-er person (Attorney) whom the person with schizophrenia trusts to MANAGE THEIR FINANCES WHEN THEY CANNOT DO IT INDEPENDENTLY. This agreement might specify who will be in control of their money and how much power they will have (e.g., their personal bank accounts access or the ability to make payments on their debts).
Housing
Individuals with schizophrenia require a RELIABLE LIVING SPACE. The choice of place should depend on their ability to take care of themselves, as well as the necessary amount of supervision. Before taking a decision, try to answer the following questions:
• Is your loved one able to take care of themselves?
• How much support is needed to assist them with their daily activities?
• Does your loved one struggle with drug or alcohol dependence?
• How much supervision does your loved one need with their treatment?
Even when you can answer these questions clearly, making a decision about the living arrangements of your loved one CAN BE A DAUNTING TASK. It is normal to feel guilt when thinking about the possibility of placing them in an institution.
As we mentioned in the first chapters of this guidebook, the current trend in the treatment
of persons with schizophrenia is to KEEP THEM IN THE NURTURING ENVIRONMENT
OF THEIR FAMILY AND TO REINTEGRATE THEM AS MUCH AS POSSIBLE INTO SOCIETY. As such, the prospect of placing your loved one in an institution is rather the exception than the norm. However, in certain cases, there may be more benefits in treating them in a specialized facility.
Living with family is most successful in the following cases:
• The person with schizophrenia has high functionality levels, is able to sustain friendships, and engages in activities outside the home.
• The interaction between family members happens in a calm manner.
• Individuals with schizophrenia have the intent of using the available support services.
• There is not any negative impact on the life of young children living in the home.
Living with family is not recommended in the following cases:
• The main caregiver is themselves ill, single, or of old age.
• The individual’s schizophrenia is critical and would impede an ordinary family life.
• The situation induces stress in the relationship or causes children to experience
fear and resentfulness in their home.
• The majority of family events revolve around the member with schizophrenia.
• There are no support services available
MAKE THE DECISION TOGETHER with your loved one and the medical team
involved in their treatment. They can offer you advice regarding the specialized treatment facilities in your area.
References
- Healthy Living: Organising Your Time [In-ternet]. Living With Schizophrenia. [cited 2021 May 8]. Available from: https://living-withschizophreniauk.org/information-sheets/healthy-living-organising-your-time/
- Clarke J. Living With Schizophrenia [Inter-net]. Verywell Mind. [cited 2021 Jun 16].
- Budziszewska MD, Babiuch-Hall M, Wielebska K. Love and Romantic Rela-tionships in the Voices of Patients Who Experience Psychosis: An Interpretive Phe-nomenological Analysis. Front Psychol [Internet]. 2020 [cited 2021 May 19];11. Available from: https://www.frontiersin.org/articles/10.3389/fpsyg.2020.570928/full
- Hengeveld M. Job Hunting With Schizo-phrenia [Internet]. The Atlantic. 2015 [cited 2021 May 19]. Available from: https://www. theatlantic.com/business/archive/2015/07/job-hunting-with-schizophrenia/395936/
- Rauh S. Working With Schizophrenia [Inter-net]. WebMD. [cited 2021 May 19]. Available from: https://www.webmd.com/schizophre-nia/features/working-with-schizophrenia
- Tiihonen J, Haukka J, Taylor M, Haddad PM, Patel MX, Korhonen P. A nationwide co-hort study of oral and depot antipsychotics after first hospitalization for schizophrenia. Am J Psychiatry. 2011 Jun;168(6):603–9.
- Brady KT, Sinha R. Co-occurring mental and substance use disorders: the neuro-biological effects of chronic stress. Am J Psychiatry. 2005 Aug;162(8):1483–93.
- Wright H. Caregiver and Schizophrenia: How to Handle the Psychosis [In-ternet]. Caregiver.com. 2017 [cited2021 May 21]. Available from: https://caregiver.com/api/content/5f180622-35a6-11e7-8b89-0aea2a882f79/
- Mueser KT, Gingerich S. The Complete Family Guide to Schizophrenia: Helping Your Loved One Get the Most Out of Life. New York: Guilford Press; 2006.
- Birchwood M, Spencer E, McGovern D. Schizophrenia: early warning signs. Adv Psychiatr Treat. 2000 Mar;6(2):93–101.
- Helping Someone with Schizophrenia – HelpGuide.org [Internet]. https://www.helpguide.org. [cited 2021 May 8]. Available from: https://www.helpguide.org/articles/mental-disorders/help-ing-someone-with-schizophrenia.htm
- Risk of Suicide [Internet]. NAMI: Nation-al Alliance on Mental Illness. [cited 2021 May 17]. Available from: https://www. nami.org/About-Mental-Illness/Com-mon-with-Mental-Illness/Risk-of-Suicide
- Elbogen EB, Wilder C, Swartz MS, Swan-son JW. Caregivers as Money Manag-ers for Adults with Severe Mental Illness: How Treatment Providers Can Help. Acad Psychiatry. 2008 Mar 1;32(2):104–10.
SCHIZOPHRENIA: MYTHS vs TRUTHS
You might already have some preconceptions about schizophrenia, but do you know the myths from the truths? Explore common myths about schizophrenia and the trut
more…SLEEP YOURSELF HEALTHY
During the brain’s activity when we are awake, potentially toxic waste products are produced and accumulated in the brain. For healthy brain functioning and men
more…