Schizophrenia in view
In this section
What is schizophrenia?
Schizophrenia is a chronic mental disorder that impacts the way a person JUDGES, PERCEIVES, AND BEHAVES. Individuals suffering from schizophrenia experience disruptions in how they perceive the world and express themselves. They often seem to have lost touch with reality and this would cause significant distress for them, their family members, and their friends. People living with schizophrenia may have difficulties discerning reality from fantasy. They may worry that others are reading their mind, secretly planning to harm them. They may also hear, see, touch, or feel things that are not there. Other times, they may experience difficulties in feeling, reading, and expressing emotions. As their thinking process becomes affected, they may have trouble concentrating or making decisions. Also, activities that they used to enjoy may not bring them pleasure anymore. These symptoms have a serious impact on their everyday activities and relationships. Schizophrenia is less common than other
mental disorders and affects an approximate number of 24 MILLION people around the world or 0.32% of the world population. Schizophrenia occurs at similar rates in all genders, races, ethnic groups, and economic backgrounds.
When do the symptoms occur?
The first schizophrenia symptoms typically occur during the patient’s late teenage years and early thirties. Men and women are equally likely to develop the disorder. In men, symptoms tend to appear earlier, from their late adolescence to emerging adulthood. Women are at higher risk of experiencing symptoms during their late 20S to early 30S. This disorder may also appear around the age of 45–50. Due to its wide range of manifestations, SCHIZOPHRENIA IS ONE OF THE MOST COMPLEX MENTAL DISORDERS.
Although schizophrenia is a chronic disorder, it can be treated with medication.
In the long term, the lives of people with this condition may be substantially improved
by psychotherapy and psychosocial treatments.
What are the risk factors for schizophrenia?
We’ve learned a great deal about schizophrenia in the last few decades.
However, 008C95.
Researchers believe that it could be caused by an interaction between GENES AND ENVIRONMENTAL FACTORS.
Genes play a very important role in schizophrenia. Studies suggest that many different genes may be involved. However, a single gene is not the cause of the disorder. It is also clear that genes are not the direct cause of schizophrenia. Rather, they foster individuals to be vulnerable to the development of this disease. There is also evidence of a genetic predisposition.
Sharing the same DNA as someone with schizophrenia increases the likelihood of developing it. If that relative is close one, the risk becomes 15 times higher. But if that relative is an identical twin, the risk increases to around 50%
Developmental and environmental factors include poverty, stress, viruses, toxins, nutritional problems before birth, as well as pregnancy and birth complications. Living in an area with a dense population or having a familial background defined by abuse and trauma, high intelligence deficient, and distressing encounters with bullying may also represent risk factors. Adolescence is considered a turning point in the development of schizophrenia. During this body development period, the brain goes through a series of changes as it matures. In the case of a vulnerable person, these changes may trigger psychotic episodes.
Drug abuse is also seen as a risk agent in the development of schizophrenia, especially in adolescence. Cannabis, for example, combined with other risk factors mentioned above, seems to be directly involved in the development of the disorder.
How does schizophrenia influence the brain?
Schizophrenia has a wide range of symptoms. In order to understand these symptoms, we first must take a look at what happens in the brain of a person with the disorder. Research has shown that in people with schizophrenia brain cells work and communicate with each other differently.
– The role of neurotransmitters
Neurotransmitters are chemical messengers that carry information between brain cells. Having too much or too little of these messengers has an impact on how the brain functions. One of the most studied neurotransmitters in schizophrenia is DOPAMINE. Also called the “feel good” neurotransmitter, dopamine plays an important role in thinking, perception, and motivation. In schizophrenia, too much dopamine in some parts of the brain may lead to hallucinations or delusions. On the other hand, too little dopamine in other parts of the brain may explain the lack of motivation and energy that is typical in schizophrenia.
Other neurotransmitters, such as GABA , glutamate , and serotonin (also called “the happy chemical”)
may also play an important role. These changes may explain symptoms such as memory lags, trouble shifting between tasks, or feeling distracted. They may also be the cause of making bad judgement calls or failing to predict consequences.
– The default mode network
Some areas in our brain become active when we let our thoughts run free. This enables us to daydream and process thoughts and memories. Scientists call this the “default mode”, and the brain areas that are involved the “default mode network”. In people with schizophrenia, THESE AREAS ARE ALMOST CONTINUOUSLY IN A STATE OF OVERDRIVE.
This makes it difficult for them to pay attention or remember information.
What are the symptoms of schizophrenia?
POSITIVE SYMPTOMS
Positive symptoms (often called “psychotic symptoms”) are thoughts and behaviours which are not present in healthy people. Several positive symptoms may be present at once. They include:
HALLUCINATIONS: hearing, seeing, or feeling things that are not actually real and cannot be perceived by others. They can include hearing sounds, music, whispers or voices, seeing objects, flashes, or persons, sensing textures or objects, tasting or smelling things. The most common hallucinations involve hearing commenting voices, usually as a dialogue, which are often criticizing or threatening. These voices may also tell the patient to do things he/she otherwise wouldn’t do.
DELUSIONS: uncorrectable false beliefs that are not shared by others and may appear as bizarre. Individuals with schizophrenia frequently believe they are being persecuted or spied on. Other times they believe that others can read their thoughts, or that they have special powers or abilities. Several types of delusions can occur at once.
DISORGANIZED THOUGHT AND SPEECH: involves confused and disordered speech and thinking. Patients often stop in the middle of a sentence. They may also put together words without any logical meaning, talk about things that are irrelevant to the topic, or jump from one idea to another. This way, their speech may become hard to understand.
BIZARRE BEHAVIOURS: could manifest in several forms, from childlike silliness to unexpected agitation. Other times, the patient may take a bizarre posture, or use excessive movement. He/She may also resist instructions, or show a complete lack of response.
NEGATIVE SYMPTOMS
Positive symptoms (often called “psychotic symptoms”) are thoughts and behaviours which are not present in healthy people. Several positive symptoms may be present at once. They include:
REDUCED EXPRESSION OF EMOTIONS (also called “BLUNTED AFFECT”or “FLAT AFFECT”): this affects speech, facial expressions, and even movement. The person’s speech becomes flat, with a dull, monotone voice. Their face shows no emotion, and they may even avoid eye contact.
REDUCED ABILITY TO SPEAK (also called “ALOGIA”): speech is reduced and becomes very poor. Replies may be delayed, using short or one-word sentences. This creates the impression of inner emptiness.
REDUCED ABILITY TO EXPERIENCE PLEASURE (also called “ANHEDONIA”): little or no interest in activities that used to bring joy. These activities include listening to music, gardening, nor even eating. Feelings towards loved ones can also be affected.
LACK OF MOTIVATION (also called “AVOLITION”): a significantly diminished sense of drive and purpose. It also manifests as a lack of ability to follow through on plans. It is important to note that these manifestations are caused by the disease and not by a lack of willpower.
SOCIAL WITHDRAWAL (or “ASOCIALITY”): a decreased interest in forming close relationships with others. This leads to a significant reduction in social interactions.
COGNITIVE SYMPTOMS
Cognitive symptoms affect thinking and mood and lead to worsening performance at school and work. They typically appear before the positive symptoms and are often still present after the positive ones have diminished. Cognitive symptoms include problems with ATTENTION, CONCENTRATION, and MEMORY.
People with schizophrenia have difficulties learning new things, or processing information to make decisions. They may also have trouble focusing and paying attention, often because of
hallucinations. Because they are unable to respond properly to others, they often communicate as little as possible. Cognitive symptoms make it more difficult to perform everyday activities. As a consequence, they can be one of the most debilitating aspects of schizophrenia. Often, people with schizophrenia are not aware that they are suffering from the disorder. This lack of insight, also called “anosognosia”, can make their treatment and care much more challenging.
AFFECTIVE SYMPTOMS
Alongside the types of the aforementioned symptoms, people with schizophrenia frequently
exhibit affective symptoms such as depression and anxiety. Depression can be present in up to 80% of people with schizophrenia and can have a wide range of negative consequences: it increases the risk of a relapse, and it leads to worse social functioning as well as poorer life quality. Depression also increases suicide risk: almost two-thirds of people with schizophrenia who take their lives do so while having depressive symptoms. Around half of people with schizophrenia have suicidal thoughts and mood problems, either as a symptom of the illness
or due to the stress and social issues caused by schizophrenia. Furthermore, around 30% have obsessive-compulsive symptoms, manifested as recurrent, intrusive, and unwanted thoughts that cause significant distress and depression.
Schizophrenia reveals three phases
The schizophrenia course depends on several factors: when the symptoms begin, how severe they are, and how long they last. Early symptoms often appear progressively and become more severe and evident over time.
Individuals may experience periods of symptom worsening and symptom improvement. The periods of symptom worsening are known as flares or relapses. By using treatment, the majority of such symptoms can decline or disappear (particularly the positive ones). Remission relates to a period without symptoms or mild symptoms only.
Although the course of the illness varies from one person to another, it can be divided into three distinct phases: PRODROMAL, ACTIVE, and RESIDUAL.
Prodromal phase
Prodromal means “before the disease”. In this phase, which may last 2–5 years, individuals undergo chang- es that become noticeable to family and close friends. These changes include memory and concentration problems, or unusual behaviour and ideas. They may also exhibit disorganized communication and decreasing interest in daily activities. In adolescents, these changes are often overlooked because they are considered normal for this period. Looking back, these symptoms are easier to interpret as warning signs. However, at the time, it would have been extremely difficult to tell them apart from the usual signs of puberty.
Active phase
This phase is characterized by the appearance of psychotic symptoms such as hallucinations, delusions, and/or disorganized thinking and speaking, but also depression or flat affect. The presence of these symptoms is called “psychosis”, and its period of manifestation is called a “psychotic episode”. The symptoms may appear gradually or suddenly. In most cases, the cause remains unknown. Scientists think that the first appearance of psychotic symptoms (also called “the first break”) may be caused by stress. Patients and their family members usually seek professional help during this phase.
Residual phase
It depicts the period of 6–18 months following the active phase. In this phase, many of the characteristic psychotic symptoms diminish. However, some residual symptoms, such as hallucinations or functional im- pairment, may remain. Positive symptoms may also be replaced by negative symptoms, for example, lack of energy and withdrawal from society. In many cases, patients begin to recognize their symptoms in this period and start to learn how to manage them.
How does schizophrenia progress?
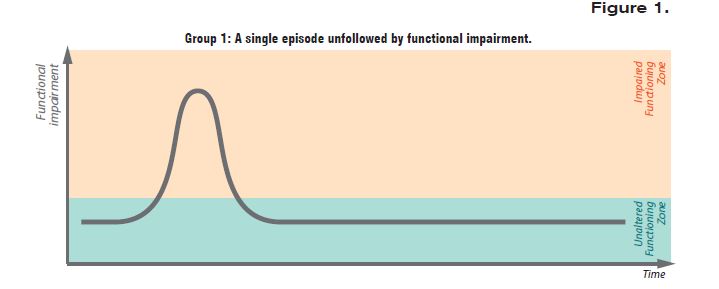
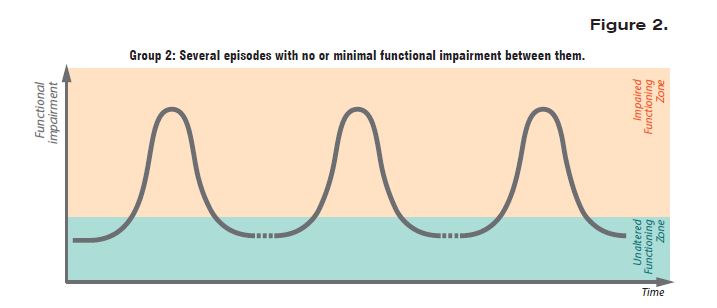
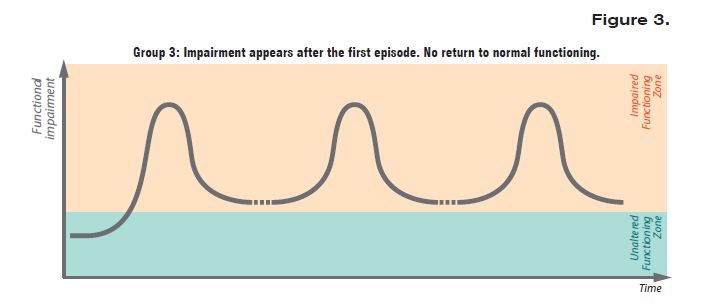
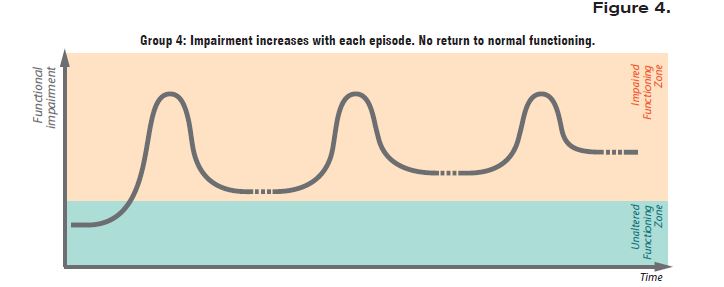
Although the illness affects every patient differently, according to research in the field, the course of the illness usually follows one of the typical forms illustrated within the next four schematic representations of the possible course of schizophrenia and its impact on patients’ normal functioning.
As Figure 1 below shows, after an acute first episode with psychotic symptoms, 22 % of those affected may experience remission, without recurrence or functional impairment in the future.
Research reveals that in 35% of the cases, the illness progresses in an episodic manner, with several psychotic episodes in the following years, as is shown in Figure 2 below. These episodes are often triggered by increased levels of stress. In some cases, there is a complete remission between individual episodes, with regained functionality.
In about 8% of those affected, there is partial remission, with diminished but persistent symptoms, as Figure 3 shows. These may include psychotic symptoms, negative symptoms, cognitive disturbances, and loss of normal functioning.
In other approximatively 35% of cases, the illness worsens progressively, and episodes cannot be identified separately. For a visual representation, please see Figure 4 below.
References
- World Health Organization. (www.who.int) Webpage: Schizophrenia. 2022.
- Lewis SW, Buchanan RW. Fast Facts: Schizo- phrenia, Fourth Edition. Health Press; 2015.
- James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet. 2018 Nov 10;392(10159):1789–858.
- Gaebel W, Wölwer W. Themenheft 50 “Schizophrenie.” Robert Koch-Institut; 2010.
- Lindamer LA, Lohr JB, Harris MJ, McAdams LA, Jeste DV. Gender-relat- ed clinical differences in older patients with schizophrenia. J Clin Psychiatry. 1999 Jan;60(1):61–7; quiz 68–9.
- Roberts LW, Hales RE, Yudofsky SC. The American Psychiatric Associa- tion Publishing Textbook of Psychiatry. Seventh Edition. American Psychiat- ric Association Publishing; 2019.
- National Institute of Mental Health. Schizophrenia [Internet]. [cited 2020 Oct 4].Available from: https://www.nimh.nih.gov/health/topics/schizophrenia/index.shtml#part_145430
- Gaebel W, Hasan A, Falkai P. S3-Leitlinie Schizophrenie. Berlin: Springer-Verlag; 2019.
- Cunningham T, Hoy K, Shannon C. Does childhood bullying lead to the development of psychotic symptoms? A metaanalysis and review of prospective studies. Psychosis. 2016 Jan 2;8(1):48–59.
- Schizophrenia – Mental Health Disorders [Internet]. Merck Manuals Consumer Ver- sion. [cited 2020 Oct 4]. Available from: https://www.merckmanuals.com/home/ mental-health-disorders/schizophrenia-and-related-disorders/schizophrenia
- Ernest, D., Vuksic, O, Smith-Shepard, A., Webb, E. Schizophrenia. An information guide. Canada. Library and Archives Can- ada Cataloguing in Publication; 2017.
- Conley RR, Ascher-Svanum H, Zhu B, Faries D, Kinon BJ. The Burden of Depressive Symptoms in the Long-Term Treatment of Patients With Schizophrenia. Schizophr Res. 2007 February; 90(1-3): 186–197
- Harkavy-Friedman J. Risk Factors for Suicide in Patients With Schizophre- nia [Internet]. Psychiatric Times. [cited 2021 Jun 16]. Available from: https://www.psychiatrictimes.com/view/risk-fac- tors-suicide-patients-schizophrenia
- Tezenas du Montcel C, Pelissolo A, Schürhoff F, Pignon B. Obsessive-Com- pulsive Symptoms in Schizophrenia: an Up-To-Date Review of Literature. Curr Psychiatry Rep. 2019 Jul 1;21(8):64.
- Corcoran C, Walker E, Huot R, Mittal V, Tessner K, Kestler L, et al. The stress cascade and schizophrenia: etiology and on- set. Schizophr Bull. 2003;29(4):671–92.
- American Psychiatric Association. The American Psychiatric Association Practice Guideline for the Treatment of Patients With Schizophrenia. Third Edition. American Psychiatric Association Publishing; 2020.
- Andresen R, Oades L, Caputi P. The experience of recovery from schizophrenia: towards an empirically vali- dated stage model. Aust N Z J Psy- chiatry. 2003 Oct;37(5):586–94.
- Andreasen NC, Carpenter WT, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry. 2005 Mar;162(3):441-9.
- Bäuml J. Psychosen aus dem schizophrenen Formenkreis: Ein Ratgeber für Patienten und Angehörige. Berlin Heidelberg: Springer-Verlag; 2013.
- Schizophrenia.com. Schizophrenia Facts and Statistics. (http:// schizophrenia.com/szfacts.htm)
SCHIZOPHRENIA: MYTHS vs TRUTHS
You might already have some preconceptions about schizophrenia, but do you know the myths from the truths? Explore common myths about schizophrenia and the trut
more…SLEEP YOURSELF HEALTHY
During the brain’s activity when we are awake, potentially toxic waste products are produced and accumulated in the brain. For healthy brain functioning and men
more…