Therapeutic amends
In this section
Although at the present time schizophrenia does not have a known cure, the outlook for individuals living with this illness is in a CONSTANT STATE OF IMPROVEMENT. For most patients, the treatment of schizophrenia involves a combination of medication and talking therapy, accompanied by social training that helps them reintegrate into society. Throughout the crisis periods or intervals of time accompanied by severe symptoms, the need for hospitalization may occur in order to ensure safety, appropriate nutrition, sufficient sleep, and basic hygiene.
Schizophrenia calls for LIFELONG TREATMENT, despite the alleviation of symptoms. In many cases, the management of patients with schizophrenia is handled by a treatment team, led by an experienced psychiatrist. The team may also be comprised of a psychologist, a psychiatric nurse, a social worker as well as a case manager which would coordinate care. Given the complexity of the disease and the fact that every person is different, there is NO “ONE-SIZE-FITS-ALL” TREATMENT. It is important to take the time to explore all options and develop an individually tailored treatment plan that works best for your loved one. The treatment objective is to reduce the symptoms, decrease the likelihood of a relapse, and increase the quality of life.
The importance of a healthy lifestyle
There are several reasons a healthy lifestyle is especially important for people with schizophrenia. Living a healthy, active life may be challenging for them because of their symptoms, such as lack of drive, or medication side effects. Also, they are more likely to suffer from an assortment of health problems, namely heart disease, stroke, cancer, and diabetes. In fact, over 75% of people with schizophrenia will also have a chronic physical condition. This can be attributed to certain lifestyle choices, such as smoking or having a poor diet, but also to the side effects of antipsychotic medication.
Smoking is a major problem that affects around 60%of people with schizophrenia, compared to 25% of people without the illness. While people with schizophrenia often use smoking as a form of self-medication, there is no scientific evidence that smoking improves their symptoms. On the contrary, there is a wealth of evidence on the detrimental effects of smoking on general health. Thereby, it is critical for people with schizophrenia to give up smoking. Another major issue is weight gain. This can be caused by a sedentary lifestyle, enabled by not having a job and the tendency to live a life that is less engaging physically, but it can also be a side effect of antipsychotic medication.
Medication
Medications are the cornerstone of schizophrenia treatment. Although there are several different treatment options and approaches in schizophrenia, medication is an elementary part of all of them. There is practically no schizophrenia treatment without medication. The most commonly prescribed drugs in schizophrenia are ANTIPSYCHOTIC MEDICATIONS.
Types of medication
As you remember from the first chapter of this guidebook, the neurotransmitter dopamine plays an essential role in schizophrenia. It is believed that in persons with schizophrenia, the AMOUNT OF DOPAMINE is TOO LOW in areas of the brain that are responsible for attention and information processing, and TOO HIGH in areas responsible for imagination and emotions. The antipsychotic medication works by CONTROLLING the amount of dopamine and other messenger substances in the brain. These medicines reduce psychotic symptoms, allowing the person you care for to function and to adjust better. Antipsychotic medications can be categorized into two groups:
TYPICAL ANTIPSYCHOTICS (also called first-generation agents)
They were introduced in the 1950S and made it possible for many people with schizophrenia to leave the hospital and return to their families and society. However, although these first-generation agents were able to control psychotic symptoms, they also caused unpleasant side effects that reduced adherence to treatment. This prompted the development of newer agents, with a lower risk of adverse events.
ATYPICAL ANTIPSYCHOTICS (also called second-generation agents)
First introduced in the 1990S, they have different mechanisms of action than first-generation agents, are better tolerated, and have the potential to lead to better long-term results. Atypical antipsychotics are more effective in preventing relapses, as well as in treating the negative and cognitive symptoms of schizophrenia. Some of the newer atypical antipsychotics discovered in the last few years have shown very promising results regarding the treatment of negative symptoms.
Both groups include many different agents with different potencies, meaning that a low-potency drug will require a higher dose to achieve the same effect as a high-potency drug with a lower dose. Antipsychotics are available in both ORAL and INJECTABLE forms. Most frequently, long-term treatment is achieved with oral medication, taken 1–3 TIMES a day. Some antipsychotics can be administered in the form of QUICK-ACTING INJECTIONS, which are especially useful in emergency situations. There are also LONG-ACTING (so-called depot) injectable antipsychotics that provide an effective alternative to persons who struggle with taking their oral medication regularly. These injections can be given EVERY FEW WEEKS, enabling a more consistent, long-term symptom relief, and are just as effective in controlling the symptoms as oral medication.
In the event of a PSYCHOTIC EPISODE, treatment with medication is started IMMEDIATELY. Most often, antipsychotics are administered in the form of injections, aiming to control the symptoms in a quick, safe, and effective manner. The goal of this treatment is to try to get the person back to normal functioning as soon as possible. This involves calming the agitated, violent, or disruptive patient, minimizing the danger to self and others, and achieving a smooth transition from injections to long-term oral treatment. After the FIRST PSYCHOTIC EPISODE, antipsychotic medication is given as MAINTENANCE THERAPY for at least 12–18 MONTHS in order to prevent further episodes. For people with SCHIZOPHRENIA IN REMISSION, MAINTENANCE THERAPY is given for at least TWO YEARS.
Within CHRONIC SCHIZOPHRENIA, when anxiety and depression are present and antipsychotics alone are not able to adequately reduce symptoms, they are sometimes combined with other types of medication such as ANTI-ANXIETY DRUGS, ANTIDEPRESSANTS, and MOOD STABILIZERS. In case of anxiety and insomnia, the most commonly used drugs are BENZODIAZEPINES, but most often they are recommended for a short period of time. In certain cases, different types of antipsychotics (for example a tablet and a depot injection) may be combined to keep the symptoms under control. Certain side effects of antipsychotics are also kept under control using other types of medication (see below). When selecting a particular medication, the psychiatrist treating the person you care for must consider a multitude of factors.
These include your loved one’s symptoms, response to previous medication, and compliance; the pattern and severity of the illness; drug interactions, adverse reactions, dosage, and the presence of other diseases. It is important to remember that every individual has a varied response to the medications administered for schizophrenia, and the time frames required to get different symptoms under control may be lengthy. While feelings of anxiety or aggression can be controlled in a matter of hours, other symptoms, such as hallucinations and delusions, may take several weeks to improve. In around 10–30% of cases, there is little improvement in symptoms even after trying two or more different antipsychotics. These persons are said to have TREATMENT-RESISTANT SCHIZOPHRENIA.The doctor treating your loved one may experiment with separate drugs and varying doses over time in order to reach the preferred result. The aim is to develop a personalized treatment that keeps the symptoms under control.
Side Effects
Side effects can be a result of both typical and atypical antipsychotics, however, it may be that some individuals will not experience them at all, while their severity may also vary for each person.
Certain antipsychotics have a sedative effect, SLOWING DOWN BRAIN ACTIVITY. This effect is more frequent with first-generation antipsychotics and may be confused with negative symptoms such as avolition, withdrawal, and lack of motivation. Sedation can be troublesome for persons with schizophrenia who are trying to reintegrate into society and can also interfere with their treatment. They describe it as LIVING IN A GLASS CASE, not being able to actively participate in life. The doctor treating your loved one may be able to reduce the sedative effect of antipsychotics by lowering the dose, changing to a single bedtime dose, or switching to a less sedating medication.
A relatively common side effect of antipsychotics is a syndrome called akathisia, characterized by a state of RESTLESSNESS accompanied by an URGENT CRAVING FOR MOVEMENT. In severe cases, persons exhibiting the syndrome feel an irresistible urge to move around and a mounting sense of tension when required to stand still. Akathisia causes severe distress, even leading to suicidal thoughts. The syndrome is caused mainly by first-generation antipsychotic drugs, but it can also be caused by newer ones. It occurs especially in the first few weeks of treatment but can become persistent if it is not addressed. Typical antipsychotics are known to aggravate the possibility of side effects that interfere with the ability to move and speak.
These include SHAKING, TREMBLING, MUSCLE TWITCHES, and MUSCLE SPASMS. They can also cause intense muscle stiffness, called dystonia. Up to 40% of the patients treated with typical antipsychotics can experience symptoms that are very similar to Parkinson’s disease – tremor, rigidity, slow movement, and gait disturbance. The majority of such symptoms can be rectified by reducing the dose or they can be kept in check by additional medications such as anti-Parkinson agents. One of the characteristic side effects of typical antipsychotics is a condition involving INVOLUNTARY, JERKY MOVEMENTS OF THE LIMBS, TONGUE, AND LIPS that cannot be controlled. The condition is called tardive dyskinesia and usually occurs after several years of treatment. Unlike other movement disorders caused by medication, tardive dyskinesia does not improve when lowering the dose or discontinuing treatment.
Atypical antipsychotics may also cause movement disorders, but the symptoms are usually much less severe. However, they are known to cause side effects interfering with one’s metabolism for instance WEIGHT GAIN, INCREASED BLOOD SUGAR AND CHOLESTEROL LEVELS, and OSTEOPOROSIS. For this reason, regular blood testing is recommended. Adaptations in nutrition and exercise, and potentially medication intervention, can assist in tackling these side effects. Both typical and atypical antipsychotics can cause drowsiness, an increase in body weight, blurred vision, constipation, absence of sex drive, and oral cavity dryness. Some of these side effects, blurred vision, for example, may improve in time with no intervention.
Others are usually countered by reducing the dosage, changing to a different antipsychotic, or using a specific medication for that side effect. As a caregiver, there are several things that you can do to reduce the negative impact of some of these side effects, especially in mild or moderate cases. You can help your loved one avoid gaining weight by ensuring they eat a healthy diet, avoid high-calorie foods and sweets, and work out. Muscle stiffness may be relieved by exercise, more specifically extensions and isometric exercises. Akathisia can also benefit from exercise and an active lifestyle.
The importance of compliance
Taking medication consistently is called medication compliance or adherence. Although taking medication on a consistent schedule may sound easy, complying with taking medication is usually one of the biggest challenges in the long-term treatment of schizophrenia. Studies have shown that 50–75% of people with schizophrenia take their medication inconsistently, and more than 40% stop completely during the first nine months of treatment. Compliance is especially important because antipsychotic medications are EFFECTIVE ONLY WHEN TAKEN REGULARLY AND CONSISTENTLY. When not taken regularly, their blood levels fluctuate and their efficiency becomes worse. You can find more information about compliance and what you can do to make sure your loved one adheres to their treatment in Chapter 6 of this guidebook.
Concerns you may have about medication
Individuals living with schizophrenia, as well as their families, may often worry about the antipsychotic medications administered for the treatment against the disorder. Besides being concerned about the side effects, they may also worry about the potential risk of addiction. Antipsychotic medication does not get individuals “high” and does not facilitate the formation of habits. Additionally, THEY DO NOT FOSTER THE DEVELOPMENT OF ADDICTIVE BEHAVIORS. A further misconception regarding antipsychotic medication is that it controls one’s mind, acting like a “chemical straightjacket”.
The appropriate use of antipsychotic drugs will not result in the lack of one’s free will or the “knocking out” of individuals who take them. Taking into account their side effects, individuals with schizophrenia may be unwilling to adhere to their medication. Besides, some people believe antipsychotics to not be beneficial and may want to discontinue their usage after they experience initial improvement. Their SUDDEN DISCONTINUATION SHOULD BE STRICTLY AVOIDED, as it can lead to the return of psychotic symptoms. It is essential to reduce the dose slowly. Always discuss with the medical team treating your loved one the benefits and side effects of the prescribed medication. It is IMPORTANT TO WEIGH HOW MANY SIDE EFFECTS ARE ACCEPTABLE in order to ensure that the person you care for is protected against a relapse, without jeopardizing their compliance.
Physical exercise
It is well known that physical exercise has a multitude of positive effects on the heart, lungs, muscles and joints, metabolism, and immune system. It also increases the production of “happy chemicals” in the brain, boosting our mood and overall sense of well-being. Exercise has several POSITIVE EFFECTS on the physical health of people with schizophrenia. It can reduce weight gain and the risk of heart disease and diabetes. It can also reduce the risk of osteoporosis, another possible side effect of antipsychotic medication. Besides improving general levels of fitness, exercise helps keep blood pressure down as well. Furthermore, getting plenty of physical exercises, particularly in the open air, improves sleep. This is especially important, as schizophrenia is often associated with sleep issues.
But more importantly, exercise has significant benefits for the psychological well-being of people with schizophrenia. Studies have shown that exercise substantially alleviates negative symptoms, particularly social withdrawal, lethargy, apathy, and cognitive symptoms such as poor memory and thinking skills. Getting more exercise helps to reduce stress and improves mood, motivation, and self-esteem. It also reduces depression and anxiety, while increasing energy. Furthermore, it is an excellent way to socialize, both for you and your loved one. There are many different types of exercise that your loved one can do including running, walking, swimming, weight training, etc. Each has different benefits: for instance, swimming will improve stamina, while weight training is better for bone strength.
Sports that improve aerobic capacities, such as martial arts, yoga, or dancing, were also shown to improve the symptoms and comorbidities of schizophrenia. The recommended amount of exercise in severe mental illnesses is 90–150 minutes per week of physical activity at moderate to vigorous intensity. It is important to do types of physical exercise that bring joy to your loved ones, as they are more likely to keep it up. It is also important to have a custom-made exercise plan that takes into account your loved one’s needs and is revised on a regular basis. Of all the treatment options listed in this chapter, exercise is the one in which you can get involved the most. Many exercises can be done at home, and you can contribute a great deal in finding the best workout routine for your loved ones and in helping them keep their motivation.
Psychotherapy
The goal of psychotherapy, or talking therapies in general, is to help persons with schizophrenia UNDERSTAND THEIR SYMPTOMS AND LIVE THEIR LIVES WITH LESS DISTRESS. Psychological treatments can aid individuals with schizophrenia in dealing with positive symptoms, such as hallucination or delusions. On top of that, they can help relieve several negative ones, for instance, or anhedonia Psychological apathy treatments are most effective when used in combination with antipsychotic medication.
Cognitive-behavioral therapy (CBT)
CBT, or cognitive behavioral therapy, is the most frequently recommended form of talking therapy used for treating schizophrenia. Based on the idea that our emotions are produced by our thoughts, CBT is a problem-focused approach that teaches people with schizophrenia HOW TO COPE WITH DIFFICULT SITUATIONS. By helping to identify and change negative thoughts and behavior, CBT helps deal with symptoms like delusions or hearing voices, and with social anxiety and depression.
CBT works by teaching individuals how to reform the beliefs or behaviors they might have that could be causing the experience of negative emotions. The therapy consists of two major elements: a COGNITIVE COMPONENT helping the individual to adjust their thought process when assessing a situation, and a BEHAVIORAL COMPONENT, helping the individual regulate the way they react to it.
CBT sessions typically last 50 MINUTES a week during the course of 3 TO 6 MONTHS, sometimes 12 MONTHS or more. During the sessions, the person you care for learns the effect their thoughts, feelings, and behaviors have on each other under the guidance of a therapist. With the end goal of eliminating undesired feelings, strategies for altering negative thoughts and improving one’s reactions to them are also taught by the therapist. Furthermore, the individuals learn ways of assessing whether their thoughts and perceptions are based on reality, as well as how to manage the accompanying symptoms.
CBT helps people learn how their decision-making mechanism is influenced by thoughts they have about themselves and the world surrounding them. Since insights like this are not often present in those with schizophrenia, CBT can help them gain more control over their emotions and behaviors. Another important component of CBT is psychoeducation. During these psychotherapeutic interventions, your loved one is informed about the disease and its treatment. The goal is to promote understanding of the disease and self-responsible coping. This is achieved by empathetic guidance through information and joint consideration.
Your loved one can learn how to take control of their life, co-living with the illness. In order for them to be able to cope with the disease as well as possible, they must develop a basic understanding of the background of their disease and the treatment options currently available. They must also learn how to detect relapses at an early stage and be able to act against them. By combining CBT sessions and administered medications, persons with schizophrenia are ultimately able to identify the trigger factors leading to their psychotic episodes and how to reduce or stop them.
–Mrs. B. K., mother of a young woman with schizophrenia
Family therapy
A large number of individuals are living with schizophrenia. Although the majority of family members are usually happy to provide help, taking care of someone with schizophrenia can be overwhelming for any given family. Family therapy is a means of supporting family members of a person with schizophrenia to cope better with the disease. It aims to GET EVERYONE IN THE FAMILY TO WORK TOGETHER in order to improve the situation for the person in question and the whole family. Family therapy is comprised of a succession of meetings over the span of about 6 MONTHS. The meetings have a clear structure and offer professional guidance. During these meetings, you may discuss information about schizophrenia, explore how you can support your loved one, and decide ways of working out practical problems brought about by the symptoms of schizophrenia. The main benefit of family therapy is that it offers a platform for the healing of family dynamics that could have arisen due to the illness. The sessions are also an opportunity for the collection of information regarding schizophrenia, cooperative navigation of challenges, as well as ways to enhance the expression and meeting of the needs of those involved. This type of psychoeducation has proved to be very effective in family therapy. Furthermore, family interventions for psychosis have been shown to reduce relapse rates, duration of hospitalization, and psychotic symptoms, as well as increase functionality.
–Mrs. F. M., mother of a young man with schizophrenia
Social training skills
Social skills training employs behavioral therapy to teach people with schizophrenia HOW TO COMMUNICATE THEIR EMOTIONS BETTER. This is particularly important when they experience difficulties in expressing their emotions or a reduction in social interactions. This type of training focuses on several aspects of a person’s relationship to others, from using eye contact and gestures, to managing negative emotions. This enables them to navigate their relationships better, reducing the distress and difficulty they experience when relating to their friends, family members, or coworkers. Besides improving social skills, these programs also IMPROVE THE QUALITY OF LIFE of people with schizophrenia, reducing relapse rates.
–Mr. P. F., father of a young man with schizophrenia
Electroconvulsive therapy
Although it has been around for a long time, electroconvulsive therapy (ECT) is still surrounded by several misunderstandings. It is often considered a method of “last resort” that causes a great deal of pain to the treated person. This can be attributed in part to the way it was incorrectly depicted in movies and TV shows. ECT is actually a SAFE AND EFFECTIVE METHOD that involves sending a small electric shock to the brain. This is done by placing electrodes on the scalp and delivering electric current through them for a very short time, while the person is under general anesthesia. The current causes brief, controlled brain seizures. A course of ECT therapy generally entails 2–3 treatments per week over the course of several weeks. Gradually, ECT RESULTS IN AN IMPROVEMENT OF ONE’S MOOD AND THOUGHTS. The decision to use ECT is always based on ethical considerations and requires signed consent from the patient.
While ECT is traditionally used to treat severe depression or bipolar disorder, it is sometimes used to treat schizophrenia symptoms such as delusions, hallucinations, or disorganized thinking. It is usually employed in critical cases, when medications are no longer effective, or if the treatment of schizophrenia is impeded by severe depression. In this regard, ECT is many times a life-saving intervention.
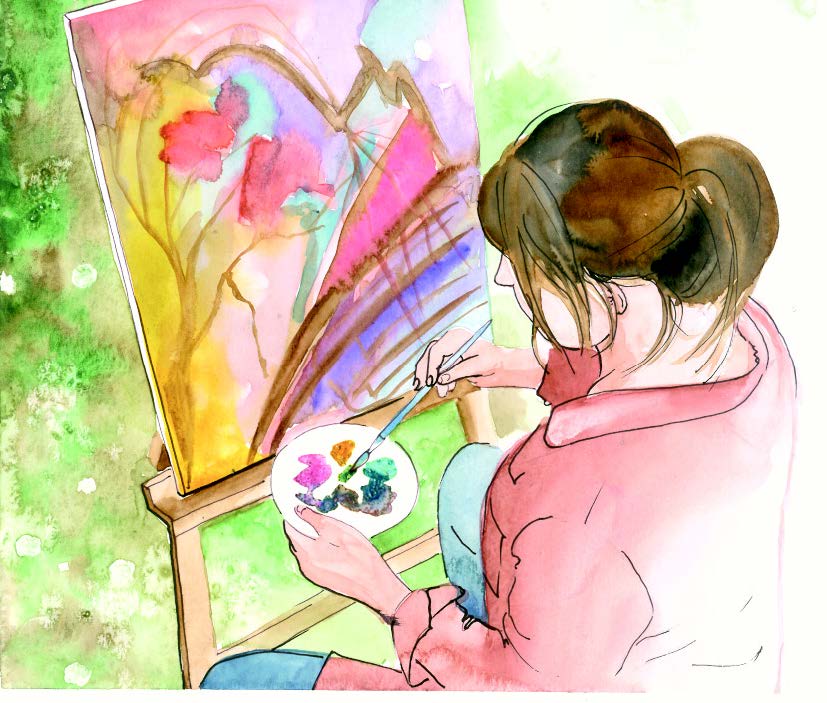
Art therapy
Art therapy, a type of psychotherapy aimed at supporting people experiencing distress, uses art as its main method of expression and communication. Art therapy encompasses a variety of methods including music, visual art, movement and dance, drama and theater, and writing. Frequently, more than one type of method is used in therapy. Art therapy is devised to FACILITATE CREATIVE EXPRESSION. Working alongside an art therapist either as an individual or in small groups can offer a new-fashioned experience of schizophrenia as well as support in the development of alternative ways to relate to other individuals. As people with schizophrenia tend to withdraw socially, art therapy makes it easier for them to engage when direct verbal interaction becomes difficult.
Art therapy may help people with schizophrenia express how they feel, particularly in cases where they find it overwhelming to discuss things or experience alienation from their feelings. Additionally, they can help face up to traumatic events from their past which could have played a part in provoking their psychotic experiences. The aim of using art therapy is to elevate one’s level of creativity, ability to express emotions, communication skills, insight, and aptness at relating to their own self or others. Art therapy empowers individuals to convey and project their experiences in their art, including the emotional, cognitive and psychotic ones and process them at a rate personally suitable to them. Even though it is not clear how and why art therapy works, there are studies suggesting that it helps people with schizophrenia control their psychosis. It also helps them to better understand symptoms such as hallucinations or delusions. Additionally, there is evidence that art therapy can facilitate recovery, particularly for individuals experiencing negative symptoms. Thus, art therapy is considered by both therapists and patients to be a beneficial and meaningful intervention.
Pets and animal-assisted therapy
Pets are known to have a positive effect on our lives. They can help ease the pain when we’re facing chronic health issues, loneliness, or depression, giving us a reason to change our focus on a sense of purpose. As a result, they have been used in therapy for centuries. Animal-assisted therapy includes animals in the treatment plan, as emotional support, or as service animals trained to assist with daily activities. Although dogs are the primary animals used, animal-assisted therapy may also use horses, cats, birds, and other animals.
The positive effect of pets has also been studied in people with schizophrenia. One study found that the presence of a dog during therapy sessions improved anhedonia, motivation, and the way the participants used leisure time. The participants’ ability to socialize and the way they viewed themselves have also shown improvements. Other studies reported improvements regarding three types of schizophrenia symptoms: positive, negative, and cognitive.
OWNING A PET HAS A SERIES OF BENEFITS on people with long-term mental health conditions: pets are often considered as important as family members, being capable of providing a secure and intimate relationship. They also have the ability to distract from distressing symptoms and upsetting experiences, and to encourage physical activity. Pets provide comfort in times when relationships with friends or family are limited or difficult. Pets also help develop routines that provide emotional and social support. By needing to be taken care of, they provide a sense of control that people with schizophrenia may not find in other relationships. Furthermore, pets can have a positive influence on the stigmatization related to mental illness, providing their owners with the feeling of being accepted. As a result, pet ownership and animal-assisted therapy may contribute to the psychosocial rehabilitation and quality of life of people with schizophrenia.
Therapeutic communities
Therapeutic communities are small cohesive groups where people can practice the basic skills of living with other people and get help while helping others. Originally developed for the rehabilitation of psychologically traumatized soldiers, therapeutic communities have been successfully used in the treatment of severe mental illnesses such as schizophrenia. They are structured around responsibility, cooperation, and communication, and participants can live in the community as residents, or take part in group meetings several times a week. The goal is to provide low-stress family-like settings for people with a mental illness, where they receive continuous support and have the opportunity to improve their social relationships and sense of purpose. In this regard, the community itself works as an instrument of therapy.
Progressive muscle relaxation
Progressive muscle relaxation (PMR) is a technique for deep relaxation based on repeatedly tightening and relaxing one muscle group after the other, synchronized with breathing. PMR has been successful-ly applied to KEEP STRESS AND ANXIETY UNDER CONTROL, relieve insomnia, and minimize certain types of chronic pain. It can also be used to reduce stress and anxiety in patients with schizophrenia, leading to an increase in subjective well-being.
Video games
Video games are a relatively new method in the treatment of schizophrenia. Although they are often perceived to promote intellectual laziness or a sedentary lifestyle, video games actually allow players to DEVELOP A WIDE RANGE OF COGNITIVE SKILLS, and they IMPROVE BRAIN PLASTICITY. It has been shown that vid-eo games – especially those which involve movement and physical exercise (called exergames) – improve the cognitive abilities and motivation of young individuals with schizophrenia. They can also improve their emotional state, mood, and social skills, and can be an appealing alternative to physical activity. Furthermore, research suggests that by playing a video game, people with schizophrenia can be trained to BETTER CONTROL VERBAL HALLUCINATIONS.
Telehealth
During the pandemic, the possibility to see your doctor in person has reduced dramatically. At the same time, however, there has been a significant rise in the use of video chat applications that allowed people to see and talk to each other using their smartphones or computers. Besides enabling people to maintain contact as well as children to continue learning through online classes, these applications also allowed mildly ill patients to talk to their doctors and get the care they need while minimizing their exposure to the virus or other ill patients. Although there are some inherent limitations to this technology (mainly related to the quality of examination and the efficiency of health care delivery), we’ve witnessed the beginning of the digital transformation of the doctor-patient relationship, which provided patients essential health care access during a major public health crisis and on the long term it will probably change the way we communicate with our doctor.
Finding the right treatment
For a person with schizophrenia, finding the right treatment can often be quite a journey. A big part of this journey is EXPLORING AND DISCOVERING THE METHODS that work best for your loved one and their symptoms. It is important to be patient throughout this process. Despite the strong desire for the withdrawal of symptoms, each individual has their own path of finding what treatments are most suitable for them personally. Although the process may feel overwhelming, there is a wide range of actions available to help ease this process. The most important is TO SHARE YOUR EXPERIENCES with your treatment team. It is important for the team to have a clear understanding of the symptoms to be able to generate a treatment plan that is personally effective for your loved one.
References
- Altamura AC, Fagiolini A, Galderisi S, Rocca P, Rossi A. Integrated treatment of schizophrenia. Journal of Psychopathology 2015; 21:168-193
- Uçok A, Gaebel W. Side effects of atypical antipsychotics: a brief overview. World psychiatry: official journal of the World Psychiatric. Association (WPA) 2008. 7(1), 58–62. https:// doi.org/10.1002/j.2051-5545.2008.tb00154.x
- Caponnetto P, Polosa R, Robson D, Bauld L. Tobacco smoking, related harm and motivation to quit smoking in people with schizophrenia spectrum disorders. Health psychology research vol. 8,1 9042. 27 May. 2020, doi:10.4081/hpr.2020.9042
- Haddad PM, Brain C, Scott J. Nonadherence with antipsychotic medication in schizophrenia: challenges and management strategies. Patient Relat Outcome Meas. 2014;5:43-62. Published 2014 Jun 23. doi:10.2147/PROM.S42735
- Falkai P, Malchow B, Wobrock T. et al. The effect of aerobic exercise on cortical rchitecture in patients with chronic schizophrenia: a randomized controlled MRI study. Eur Arch Psychiatry Clin Neurosci 263, 469–473 (2013). https://doi.org/10.1007/s00406-012-0383-y
- Farholm A, Sørensen M. Motivation for physical activity and exercise in severe mental illness: A systematic review of cross-sectional studies. Int J Ment Health Nurs. 2016 Apr;25(2):116-26. doi: 10.1111/inm.12217. Epub 2016 Feb 1. PMID: 26833453.
- Jingxuan H. Art Therapy: A Complementary Treatment for Mental Disorders. Front. Psychol. 12 August 2021. https:// doi.org/10.3389/fpsyg.2021.686005
- Vancampfort D, De Hert M, Knapen J, Maurissen K, Raepsaet J, Deckx S, Remans S, Probst M. Effects of progressive muscle relaxation on state anxiety and subjective well-being in people with schizophrenia: a randomized controlled trial. Clin Rehabil. 2011 Jun;25(6):56775. doi: 10.1177/0269215510395633. Epub 2011 Mar 14. PMID: 21402653.
- Nathans-Barel I, Feldman P, Berger B, Modai I, Silver H. Animal-assisted therapy ameliorates anhedonia in schizophrenia patients. A controlled pilot study. Psychother Psychosom. 2005;74(1):31-5. doi: 10.1159/000082024. PMID: 15627854.
- Hosak L. Electroconvulsive Therapy in Schizophrenia. World J Psychiatry Ment Health Res. 2018; 2(1): 1008
- Almerie MQ, Okba Al Marhi M, Jawoosh M, Alsabbagh M, Matar HE, Maayan N, Bergman H. Social skills programmes for schizophrenia. Cochrane Database Syst Rev. 2015 Jun 9;2015(6):CD009006. doi: 10.1002/14651858.CD009006.pub2. PMID: 26059249; PMCID: PMC7033904.
- Camacho-Gomez M, Castellvi P. Effectiveness of Family Intervention for Preventing Relapse in First-Episode Psychosis Until 24 Months of Follow-up: A Systematic Review With Meta-analysis of Randomized Controlled Trials. Schizophr Bull. 2020 Jan 4;46(1):98-109. doi: 10.1093/schbul/sbz038. PMID: 31050757; PMCID: PMC6942164.
- Reeves JJ, Ayers JW, Longhurst CA. Telehealth in the COVID-19 Era: A Balancing Act to Avoid Harm. J Med Internet Res. 2021 Feb 1;23(2):e24785.
SCHIZOPHRENIA: MYTHS vs TRUTHS
You might already have some preconceptions about schizophrenia, but do you know the myths from the truths? Explore common myths about schizophrenia and the trut
more…SLEEP YOURSELF HEALTHY
During the brain’s activity when we are awake, potentially toxic waste products are produced and accumulated in the brain. For healthy brain functioning and men
more…