The Challenge of Negative Symptoms in Schizophrenia
- Negative symptoms can be difficult to recognize as part of schizophrenia, they are rarely the reason patients seek help, and treatment remains a challenge for patients with these complicated and heterogeneous symptoms1,2.
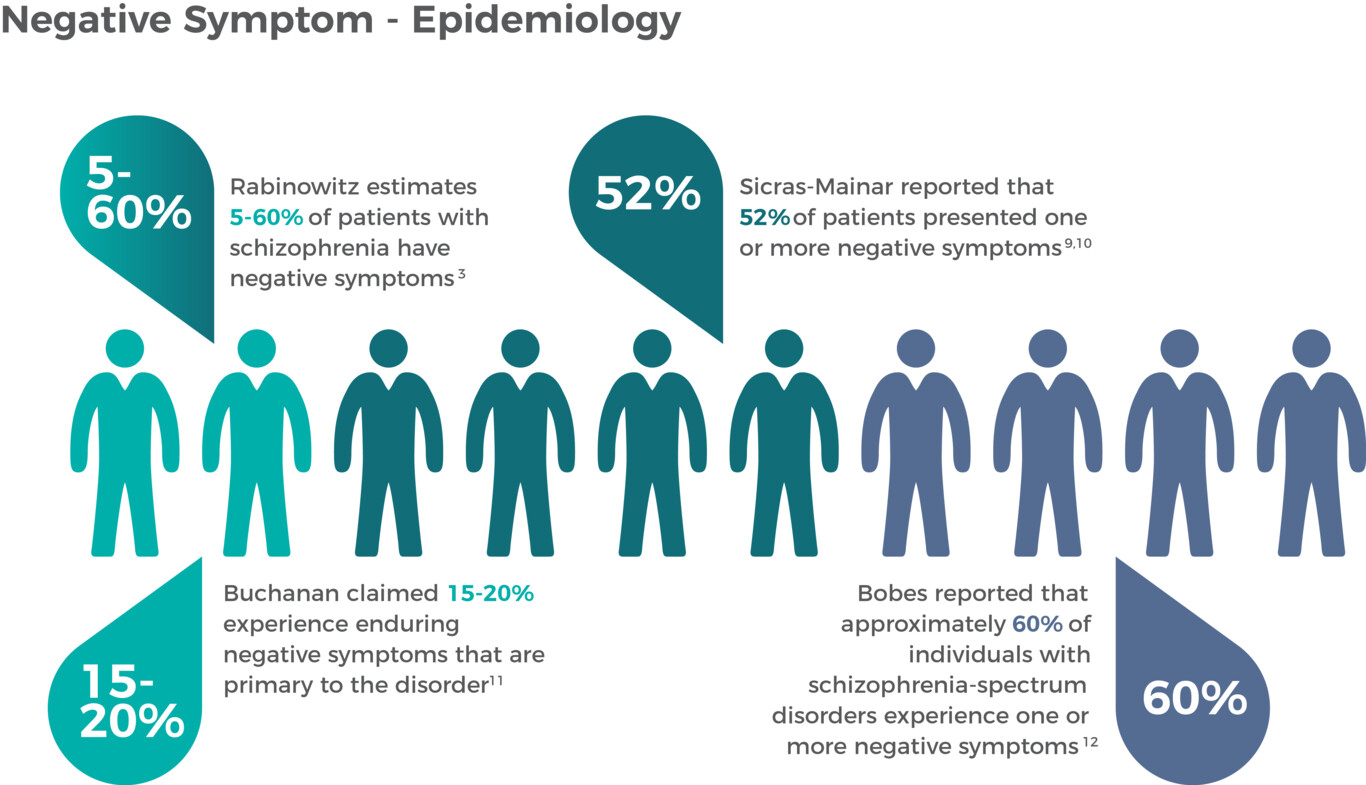
- Negative symptoms are a core symptom of schizophrenia with prevalence estimates that are wide-ranging (approximately 5%-60%) depending on the criteria applied to define the negative symptom3.
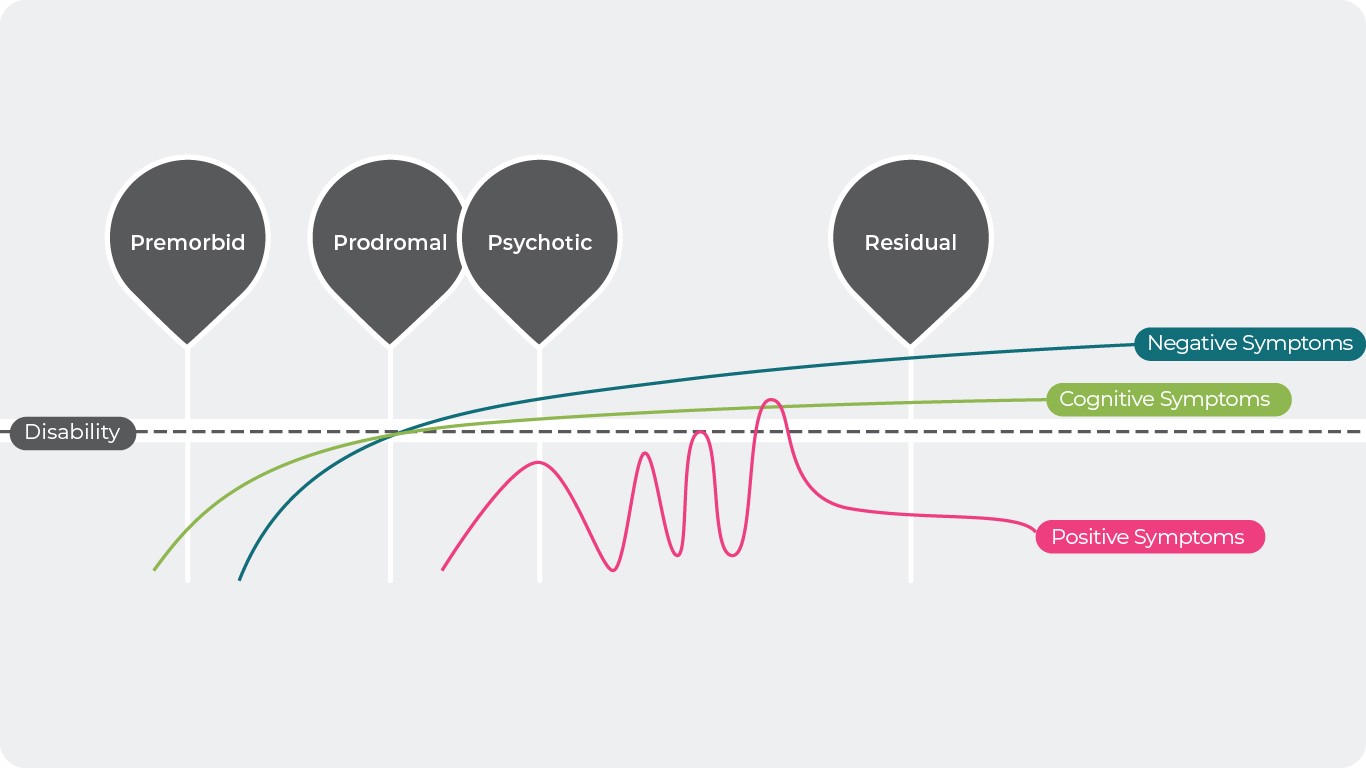
- Negative symptoms may occur earlier than positive symptoms and remain present or worsen throughout the course of the disease from the beginning (prodromal phase), to the middle (where they are interspersed with positive symptoms), until the end (residual phase)4,5.
In this section
Recognition and Prevalence of Negative Symptoms
Although negative symptoms have long been recognized as an independent symptom domain, distinct from positive symptoms, neurocognition, and social cognition, they can still be difficult to recognize. For example, significant symptom-related deficiencies in affect, motivation, communication, and social functioning might easily be mistaken for depression or cognitive difficulties1, limiting the potential to appropriately manage symptoms and support the patient. Recognizing and managing these challenging symptoms is important since negative symptoms are responsible for a large part of the long-term morbidity in patients with schizophrenia6,7. Negative symptom severity has been linked to worse outcomes in several areas of functioning, including occupational and academic performance, household involvement, social interactions and formation of lasting relationships, participation in activities, and quality of life8, which speaks to the importance of providing effective treatment to improve impairment across life’s jurisdictions.
Estimates for the prevalence of negative symptoms can vary depending on the criteria that is used to define the population. For example, in a large sample of patients from clinical trials in schizophrenia, Rabinowitz et al. found that 8.1% to 62.3% met various criteria for prominent negative symptoms; similarly, 10.2% to 50.2% met various criteria for predominant negative symptoms3.
Regardless of the criteria used, the presence of negative symptoms is very common in patients with schizophrenia. A large cross-sectional, retrospective study found that 52% of patients presented with one or more negative symptoms, with social and emotional withdrawal being the most common negative symptoms observed9,10. A separate study evaluating patients in routine clinical practice found similar results, with 61% of stabilized schizophrenia outpatients presenting with at least 1 negative symptom of moderate severity or worse; social withdrawal (48%), emotional withdrawal (42%), and poor rapport (39%) were the most common symptoms, with 19% of patients exhibiting all 5 negative symptoms12. In addition, approximately 13% of patients evaluated in this study had negative symptoms that were classified as primary negative symptoms.
When the population was limited to patients with only primary negative symptoms that are persistent or enduring (ie, deficit syndrome), prevalence estimates range from 25–30% of patients in clinical samples to 14–17% of patients in population-based samples13. Based on the collective epidemiological data, it has been estimated that the prevalence of primary, enduring negative symptoms is likely in the range of 15%-20%11.
Despite a lack of consensus regarding the prevalence of these challenging symptoms, it is clear that negative symptoms are highly prevalent and associated with significant illness burden, dictating that all clinically relevant negative symptoms should be appropriately treated to improve patient outcomes.
Presentation of Negative Symptoms Across the Disease Course5
Negative symptoms have been reported as the most common first symptom of schizophrenia14, and often manifest during the prodromal period, which precedes the first episode of psychosis and can last anywhere from a few days to years15. In fact, it has been reported that 73% of patients have negative symptoms before the onset of positive symptoms and 20% of patients experience them within weeks of experiencing positive symptoms4. However, negative symptoms can also appear during the psychotic phase of illness, so when positive symptoms are accompanied by decreased emotional expression, social withdrawal, and functional deterioration16, special vigilance for negative symptoms should also be observed. Over time, positive symptoms diminish due to treatment or the natural course of illness, and more prominent negative symptoms again emerge, with negative symptoms most prevalent in the residual phase of schizophrenia11.
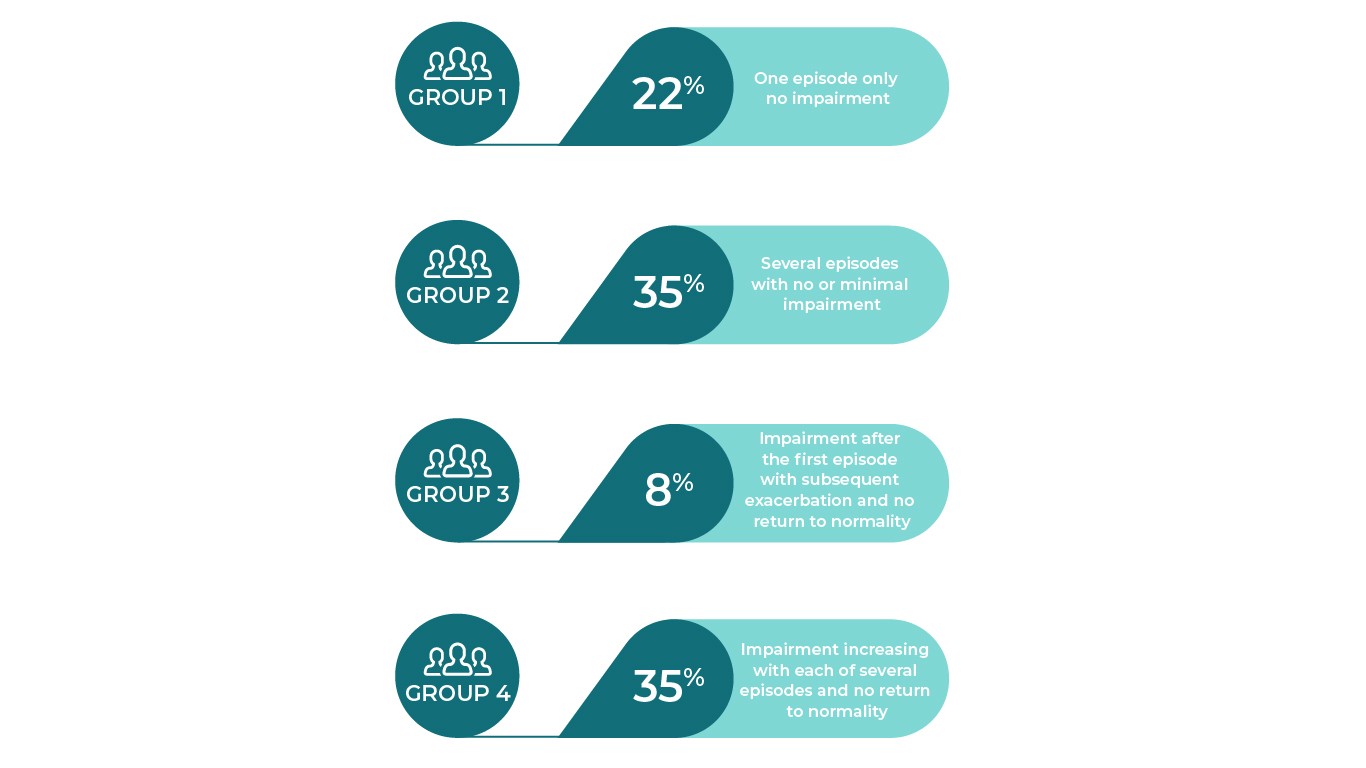
Reference: Adapted from World Health Organization. International Statistical Classification of Diseases. Online version; 2016. https://icd.who.int/browse10/2016/en#/F20-F29 Shepherd M, Watt D, Falloon I, Smeeton N. The natural history of schizophrenia: a five-year follow-up study of outcome and prediction in a representative sample of schizophrenics. Psychological Medicine. Monograph Supplement. 1989;15:1-4617.
Although there is a typical disease course and presentation of symptoms in schizophrenia, schizophrenia is by no means a homogeneous disease and not all patients will experience all stages of illness. In an attempt to classify patients according to the course of their illness pattern, 4 broad subgroups were constructed from 5-year follow-up data in a cohort of patients with schizophrenia. As shown, some patients experienced only one episode followed by recovery while others experienced frequent episodes and increasing disease severity without abatement of symptoms17. Of the patients in Groups 3 and 4, persistent florid symptoms with one or more exacerbations were noted during the follow-up period. Symptoms of auditory hallucinations; thought withdrawal, insertion and interruption; thought broadcasting; somatic hallucinations; delusional perception; and feelings or actions experienced as made or influenced by external agents (ie, first-rank symptoms) were present in 75% of patients in Group 3 and 94% of patients in Group 4 at 5 years. In the most severe group, there was a gradual increase in residual psychopathology after each exacerbation before a stable level of severe impairment was reached. Clinicians should be aware that negative symptoms can occur at any point during the course of schizophrenia; for example, at least 1 negative symptom was noted in up to 90% of patients having a first psychotic episode and 35%-70% of patients continued to have clinically significant symptoms that persisted after the initiation of treatment4,18,19.
References
- National Institutes of Mental Health (NIMH). Schizophrenia. (2017). Available at: https://www.nimh.nih.gov/health/publications/schizophrenia-booklet/index.shtml.
- Fischer, B. A. & Buchanan, R. W. Schizophrenia: Clinical Manifestations, Course, Assessment and Diagnosis. UpToDate (2017). Available at: www.up-to-date/schizophrenia.
- Rabinowitz, J. et al. Negative symptoms in schizophrenia – the remarkable impact of inclusion definitions in clinical trials and their consequences. Schizophr. Res. 150, 334–338 (2013).
- an der Heiden, W., Leber, A. & Häfner, H. Negative symptoms and their association with depressive symptoms in the long-term course of schizophrenia. Eur. Arch. Psychiatry Clin. Neurosci. 266, 387–396 (2016).
- Lieberman, J. A. Is schizophrenia a neurodegenerative disorder? A clinical and neurobiological perspective. Biol. Psychiatry 50, 884–897 (2001).
- Galderisi, S., Mucci, A., Buchanan, R. W. & Arango, C. Negative symptoms of schizophrenia: new developments and unanswered research questions. The Lancet Psychiatry 5, 664–677 (2018).
- Kirkpatrick, B., Buchanan, R. W., Ross, D. E. & Carpenter, J. A separate disease within the syndrome of schizophrenia. Arch. Gen. Psychiatry 58, 165–171 (2001).
- Foussias, G., Agid, O., Fervaha, G. & Remington, G. Negative symptoms of schizophrenia: Clinical features, relevance to real world functioning and specificity versus other CNS disorders. Eur. Neuropsychopharmacol. 24, 693–709 (2014).
- Sicras-Mainar, A., Maurino, J., Ruiz-Beato, E. & Navarro-Artieda, R. Impact of negative symptoms on healthcare resource utilization and associated costs in adult outpatients with schizophrenia: A population-based study. BMC Psychiatry 14, 225 (2014).
- Sicras-Mainar, A., Maurino, J., Ruiz-Beato, E. & Navarro-Artieda, R. Prevalence of metabolic syndrome according to the presence of negative symptoms in patients with schizophrenia. Neuropsychiatr. Dis. Treat. 11, 51–57 (2014).
- Buchanan, R. W. Persistent Negative Symptoms in Schizophrenia: An Overview. Schizophr. Bull. 33, 1013–1022 (2007).
- Bobes, J., Arango, C., Garcia-Garcia, M. & Rejas, J. Prevalence of negative symptoms in outpatients with schizophrenia spectrum disorders treated with antipsychotics in routine clinical practice: Findings from the CLAMORS study. J. Clin. Psychiatry 71, 280–286 (2010).
- Mucci, A., Merlotti, E., Üçok, A., Aleman, A. & Galderisi, S. Primary and persistent negative symptoms: Concepts, assessments and neurobiological bases. Schizophr. Res. 186, 19–28 (2017).
- an der Heiden, W. & Häfner, H. The epidemiology of onset and course of schizophrenia. Eur. Arch. Psychiatry Clin. Neurosci. 250, 292–303 (2000).
- Larson, M. K., Walker, E. F. & Compton, M. T. Early signs, diagnosis and therapeutics of the prodromal phase of schizophrenia and related psychotic disorders. Expert Rev. Neurother. 10, 1347–1359 (2010).
- Lyne, J. et al. Negative symptoms of psychosis: A life course approach and implications for prevention and treatment. Early Interv. Psychiatry 12, 561–571 (2018).
- Shepherd, M., Watt, D., Falloon, I. & Smeeton, N. The natural history of schizophrenia: a five-year follow-up study of outcome and prediction in a representative sample of schizophrenics. Psychol. Med. Monogr. Suppl. 15, 1–46 (1989).
- Mäkinen, J., Miettunen, J., Isohanni, M. & Koponen, H. Negative symptoms in schizophrenia – A review. Nord. J. Psychiatry 62, 334–341 (2008).
- Rabinowitz, J., Berardo, C. G., Bugarski-Kirola, D. & Marder, S. Association of prominent positive and prominent negative symptoms and functional health, well-being, healthcare-related quality of life and family burden: A CATIE analysis. Schizophr. Res. 150, 339–342 (2013).
Lancet Psychiatry
Negative symptoms of schizophrenia: new developments and unanswered research questions.

Negative Symptom – Epidemiology
Applying different diagnostic criteria has affected the incidence and prevalence numbers of negative symptom patients.
DownloadReferences title
NEGATIVE SYMPTOMS: DIFFERENT ORIGIN…
Primary and secondary negative symptoms may be the most important distinction in the negative symptom lexicon because of their different clinical implications.
more…OUR PRODUCT ON NEGATIVE SYMPTOMS
Negative symptoms of schizophrenia can occur as primary symptoms that are part of the underlying pathophysiology of schizophrenia or as secondary symptoms that
more…