IMPROVING REAL-LIFE FUNCTIONING IN PEOPLE WITH SCHIZOPHRENIA: FROM ASSESSMENT TO INTEGRATED TREATMENT PLANS
In this section
The symposium, entitled “Improving Real-life Functioning in People with Schizophrenia: From Assessment to Integrated Treatment” at EPA 2021 Virtual focused on presenting data in chronic and first-episode patients on predictors of clinical and functional outcomes, along with perspectives on personalised and integrated management programmes in subjects with schizophrenia and at high-risk status. The distinguished panel of speakers included Professors Carmen Moreno, Nikolaos Koutsouleris, and Paolo Fusar-Poli, moderated by Professors Silvana Galderisi and Wolfgang Gaebel. The key messages of the symposium were that:
1) The goal of schizophrenia treatment has now shifted from symptom reduction and prevention of relapses to functional recovery; however, recovery rates remain very low.1
2) Early intervention and identification of predictors of clinical and functional outcomes are essential to implement personalized and integrated treatment programmes to prevent disability and promote recovery.1
3) Stratification of subjects with high-risk status, first-episode and chronic schizophrenia using several predictors of clinical and functional outcome has the potential to contribute to early recognition, treatment, rehabilitation and personalised care, promoting prevention of disability, independent living, social inclusion and user satisfaction.1
Assessing Parameters Important for Real-life Functioning in Schizophrenia
Today there is still a significant gap between treatment goals, namely recovery and actual treatment outcomes, as stressed by Professor Silvana Galderisi, Director of the Department of Mental and Physical Health and Preventive Medicine of the University of Campania. Unfortunately, schizophrenia still remains among the top 10 causes of disability, with a life expectancy about 15-20 years shorter than in the general population.2 In order to reduce these gaps, the identification of predictors of functioning and early intervention acting on these predictors are fundamental.
In the first part of the lecture, Professor Galderisi presented the results of the Italian Network for Research on Psychoses study, which was a large cross-sectional study of 921 patients with schizophrenia living in the community.3 When analysing the results, variables relevant to the disease, personal resources and social context explained 53.8% of variance in real-life functioning.3 Among these, neurocognition exhibited the strongest, though indirect, association with real-life functioning.3 In addition, positive symptoms, disorganisation and avolition had significant direct and indirect effects, while depression had no significant association and poor emotional expression was only indirectly and weakly related to real-life functioning.3
Then Professor Galderisi presented the results of a 4-year follow-up of the same study in which five baseline variables were found to be directly associated with real-life functioning.4 These included neurocognition with everyday life and work skills, avolition with interpersonal relationships, positive symptoms with work skills, social cognition with work skills and interpersonal functioning.4
In conclusion, Professor Galderisi said that baseline variables associated with functional outcome at follow-up are not routinely assessed and targeted by intervention programs in community mental health services.4 Accordingly, routine mental health care should make greater use of cognitive training programs combined with personalised psychosocial interventions that have the goal of promoting independent living. As a result, assessment should be enlarged to include additional parameters that are highly relevant for real-life functioning.
Predicting Outcomes in Early-Onset Psychosis
Many psychiatric disorders emerge during childhood and adolescence, and 1 in 5 adolescents have a mental disorder that will persist into adulthood.5 This statement was the opening of the second lecture of the symposium presented by Professor Carmen Moreno, Associate Professor of Psychiatry at the Complutense University School of Medicine, Madrid. She noted that 10% of first-episode psychoses occur before the age of 18 years, and social and cognitive impairments typically develop before the first psychotic episode and even years before the ultra-high-risk stage.6 Thus, prevention should start much earlier in the groups at risk for schizophrenia and other psychiatric disorders.6
Notwithstanding, recognising positive psychotic symptoms and their diagnostic context in youth remains a challenge.8 For example, a large minority of subjects say they hear things others do not hear, even if they may not present with complaints of hallucinations or delusions.9 Frequently, these individuals have psychotic symptoms for an extended period before diagnosis.9 In addition, hallucinations during childhood are frequently multimodal in nature (e.g., auditory, visual), while delusions are typically vague and much less common than hallucinations during childhood.9
Professor Moreno then highlighted that negative symptoms have a large impact in first episode and those with negative symptoms are at greater risk of developing multiple treatment failures.10 Moreover, longer duration of untreated psychosis and higher symptom severity at the first episode, measured with the Clinical Global Impression Scale, significantly predicts the presence of functional deterioration at two years.11 Results of a longitudinal study further showed that only shorter duration of untreated psychosis and greater severity of baseline negative symptoms were significantly associated with greater improvement in executive function.12
Professor Moreno ended her presentation by saying that the available data indicates that treatment delay is important for overall functioning and duration of untreated psychosis has a major impact on long-term outcomes. As such, clinicians should be aware that early intervention improves prognosis, and early referral to early intervention services should be promoted.
Personalising Treatment through Machine-Learning
In his lecture, Nikolaos Koutsouleris, Professor at the Department of Psychiatry and Psychotherapy, LMU Munich, discussed the role of machine-learning in personalising treatment. First of all, it is important to note that heterogeneity of outcomes is a major point to consider in schizophrenia-spectrum disorders and can be potentially understood using advanced statistical modelling approaches.
For instance, the large European First Episode Schizophrenia Trial (EUFEST) database can help in better understanding the heterogenous nature of schizophrenia,since it has realistic outcome measures and large multi-site coverage, and is a rich set of clinical and neurocognitive data.13 Professor Koutsouleris presented data on machine learning with data from 334 patients in EUFEST that was used to develop a tool to predict poor versus good treatment outcomes (Global Assessment of Functioning [GAF] score ≥65 vs GAF <65, respectively) after 4 weeks and 52 weeks of treatment. He showed that unemployment, poor education, functional deficits, and unmet psychosocial needs predicted both 4- and 52-week outcomes, whereas previous depressive episodes, male sex, and suicidality additionally predicted poor 52-week outcomes.
He next presented a study that evaluated the efficacy of 10-Hz repetitive transcranial magnetic stimulation (rTMS) applied to the left dorsolateral prefrontal cortex for the treatment of predominant negative symptoms in schizophrenia.14 A total of 175 patients with schizophrenia with predominant negative symptoms and a high-degree of illness severity were randomised into two treatment groups: 10-Hz rTMS applied 5 days per week for 3 weeks to the left dorsolateral prefrontal cortex or sham rTMS applied similarly.14 While there was no significant difference in improvement in negative symptoms between the two groups at day 21 or through day 105, he mentioned that a subsequent analysis showed that local brain volume changes measured by deformation-based morphometry correlated with changes in negative symptom severity.15 According to Professor Koutsouleris, this demonstrates that heterogeneity in clinical response of negative symptoms in schizophrenia to prefrontal high-frequency rTMS may be related to variability in capacity for structural plasticity, particularly in the left hippocampal region and the precuneus.15
In conclusion, Professor Koutsouleris remarked that the available results demonstrate that treatment outcome prediction with single-subject accuracy may be achieved by applying machine learning to clinical and neuroimaging data. In this light, decoding outcome heterogeneity may have significant implications for design of future trials by adding machine-learning based risk stratification mechanisms.
The Challenges of Early Intervention
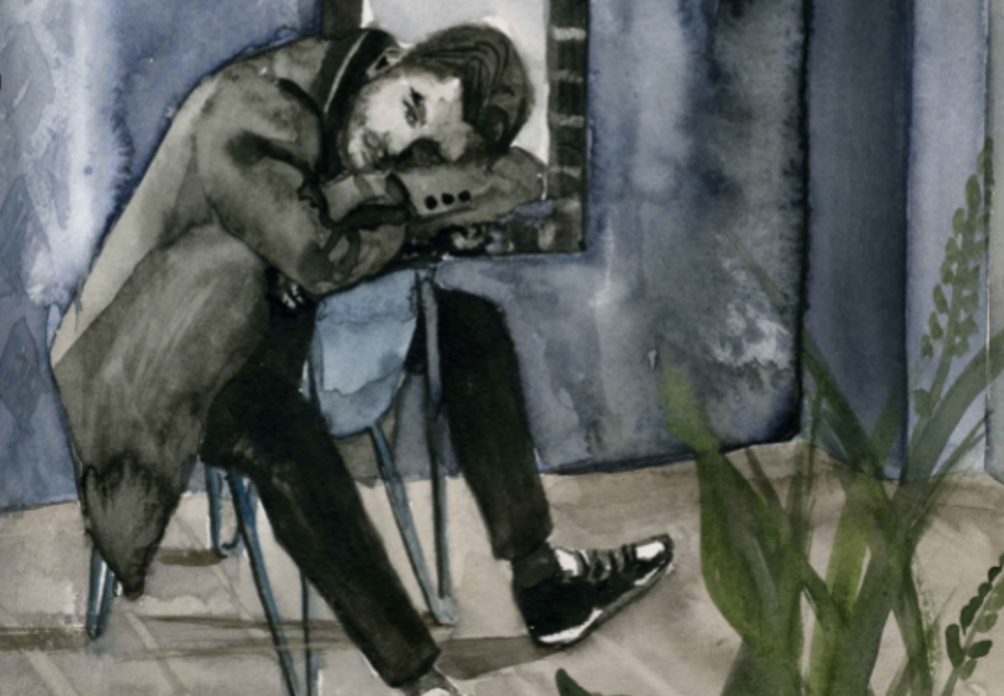
Paolo Fusar-Poli, Professor of Preventive Psychiatry at King’s College London based his talk entitled “Improving Real-life Functioning in People with Schizophrenia: From Assessment to Integrated Treatment Plans” on the case of a 17-year-old adolescent in order to illustrate the difficulties of early intervention.16
A 17-year-old boy was referred by his general practitioner to the local psychosis early-detection clinic due to a decrease in functioning and social withdrawal during the past 6 months. Prior to the age of 17, the patient had no significant medical history. He began college 6 months prior but had found the workload difficult and failed his examinations. The patient had no family history of mental disorders, and denied any current or past use of drugs. He reported that he no longer enjoyed his former interests and could not relate to people at college or to friends. No formal thought disorders were elicited, but he became socially isolated. The Structured Clinical Interview for DSM did not reveal any mental disorder, and he was not severe enough to meet entry criteria for a mood disorder. He was thus resent to his general practitioner. However, one month later he was convinced that random people looked and talked about him when he was out in public, stating that these people were probably commenting on his appearance while recording him on camera, even if he did not believe these individuals meant him harm. Acute transient psychotic disorder was diagnosed, and he was referred to a community care team, but was not accepted in care due to the fact he was underage. Also, because he was no longer psychotic, he no longer met entry criteria for treatment. He became increasingly isolated and quit college.
Professor Fusar-Poli said that he was later referred to the OASIS outreach and support programme in London where he was considered to be at high clinical risk for psychosis. Accordingly, he was given preventive treatment and ongoing monitoring and support. After 24 sessions of talking therapy and clinical monitoring, the patient returned to a healthy condition and was able to return to college and a normal social life.
Using this case as an example, Professor Fusar-Poli highlighted the current disintegration of health services at the early stages of onset of psychosis. The OASIS programme is thus a practical example of how to overcome some of these barriers by attempting to reduce ‘at-risk’ symptoms and severity, prevent the transition to psychosis and improve outcomes if psychosis develops.
References
- Maj M, et al. The clinical characterization of the patient with primary psychosis aimed at personalization of management. World Psychiatry. 20:4-33 (2021).
- Ringen PA, et al. Increased mortality in schizophrenia due to cardiovascular disease – a non-systematic review of epidemiology, possible causes, and interventions. Front Psychiatry. 5:137 (2014).
- Galderisi S, et al. The influence of illness-related variables, personal resources and context-related factors on real-life functioning of people with schizophrenia. World Psychiatry. 13:275-87 (2014).
- Mucci A, et al. Factors Associated With Real-Life Functioning in Persons With Schizophrenia in a 4-Year Follow-up Study of the Italian Network for Research on Psychoses. JAMA Psychiatry. 2021 Feb 10:e204614. doi: 10.1001/jamapsychiatry.2020.4614.
- Lee FS, et al. Mental health. Adolescent mental health–opportunity and obligation. Science. 346:547-9 (2014).
- Löffler W, et al. Validation of Danish case register diagnosis for schizophrenia. Acta Psychiatr Scand. 90:196-203 (1994).
- Sommer IE, et al. Early interventions in risk groups for schizophrenia: what are we waiting for? NPJ Schizophr. 2:16003 (2016).
- Stevens JR, et al. Psychotic disorders in children and adolescents: a primer on contemporary evaluation and management. Prim Care Companion CNS Disord. 16:PCC.13f01514 (2014).
- Larson MK, et al. Early signs, diagnosis and therapeutics of the prodromal phase of schizophrenia and related psychotic disorders. Expert Rev Neurother. 10:1347-59 (2010).
- Downs J, et al. Negative Symptoms in Early-Onset Psychosis and Their Association With Antipsychotic Treatment Failure. Schizophr Bull. 45:69-79 (2019).
- Fraguas D, et al. Duration of untreated psychosis predicts functional and clinical outcome in children and adolescents with first-episode psychosis: a 2-year longitudinal study. Schizophr Res. 152:130-138 (2014).
- Fraguas D, et al. A longitudinal study on the relationship between duration of untreated psychosis and executive function in early-onset first-episode psychosis. Schizophr Res. 158:126-133 (2014).
- Koutsouleris N, et al. Multisite prediction of 4-week and 52-week treatment outcomes in patients with first-episode psychosis: a machine learning approach. Lancet Psychiatry. 3:935-946 (2016).
- Wobrock T, et al. Left prefrontal high-frequency repetitive transcranial magnetic stimulation for the treatment of schizophrenia with predominant negative symptoms: a sham-controlled, randomized multicenter trial. Biol Psychiatry. 77:979-988 (2015).
- Hasan A, et al. Structural brain changes are associated with response of negative symptoms to prefrontal repetitive transcranial magnetic stimulation in patients with schizophrenia. Mol Psychiatry. 22:857-864 (2017).
- Fusar-Poli P, et al. A Case of a College Student Presenting With Mild Mental Health Problems. JAMA Psychiatry. 75:1298-1299 (2018).